A teenage girl with acne lesions on her forehead
Can you guess the diagnosis?
The case
A girl aged 15 years presented with a 4-month history of recurrent crusted lesions on her forehead (Figure). According to her mother, the initial lesions were blackheads from her acne. She had occasional breakouts, which evolved into more widespread hyperpigmented and crusted papules. Her mother says that the patient was increasingly preoccupied with her facial appearance and often picked at her skin in front of a mirror. The patient also acknowledged compulsive picking behaviors, especially during periods of stress or academic anxiety, often without full awareness of the behavior, and acknowledged feelings of relief afterward, followed by guilt.
A teenage girl with acne lesions on her forehead | Image credit: Author provided

On examination, the patient appeared well nourished and anxious. Her vital signs were within normal limits. On dermatological examination, there were multiple erythematous papules, linear excoriations, hyperpigmented macules, and a few shallow atrophic scars predominantly over the central forehead. The distribution was limited to easily accessible areas, with no involvement of covered sites like the scalp, trunk, or extensor surfaces. Mild comedonal and inflammatory acne were noted on the cheeks, but the extent of skin damage on the forehead was disproportionate to the severity of active acne. No vesicles, burrows, or grouped papulovesicular lesions were noted. There were no systemic symptoms, and the remainder of the skin examination was clear.
Diagnosis
Acne excoriée
Etiology and clinical findings
Acne excoriée (AE) is a skin-picking disorder (SPD) within the group of obsessive-compulsive disorder (OCD) and related disorders characterized by the compulsive manipulation of acne lesions.1 Even though the condition is common among adolescent girls, it can be seen in boys, and the age of onset may vary between 11 and 40 years.2 It is noted that younger individuals often develop new physical concerns and become more conscious of their facial appearance. Due to hormonal changes, conditions like acne can exacerbate this, and in an attempt to clear their skin, some begin picking at their lesions—often leading to acne excoriée.3
It is observed that these patients prefer the short-term relief of dealing with acne over the long-term possibility of scar-free healing of the lesion, suggesting an underlying psychiatric component in acne excoriée, such as anxiety disorder, OCD, and body dysmorphic disorder.4 Some practitioners consider acne excoriée a protective device to conceal personal failure or an appeal for help coming from persons with an immature personality who lack coping mechanisms.5
Clinically, acne excoriée presents as erosions covered by crusts as well as excoriations, ulcerations, and scars, which are often disfiguring. Studies showed that the severity of acne does not correlate with the intensity of self-excoriation in adolescent girls. Therefore, most adolescent girls with acne excoriée have mild forms of acne. However, personality traits seem to be important in those patients, often perfectionists or compulsive persons who have a higher risk of developing this disorder.6
Differential diagnosis
The differential diagnosis for excoriated or crusted facial lesions includes a wide range of psychogenic, allergic, inflammatory, and infectious conditions (Table). Acne excoriée, also known as excoriated acne, is a psychocutaneous disorder typically seen in adolescent girls, in which patients compulsively pick, scratch, or squeeze acne lesions. The result is often a pattern of excoriations, hyperpigmented macules, and shallow scars that are disproportionate to the underlying severity of the acne. Lesions are usually confined to accessible areas, such as the forehead, cheeks, and chin, while covered or hard-to-reach areas remain unaffected.7
Table. Differential Diagnosis
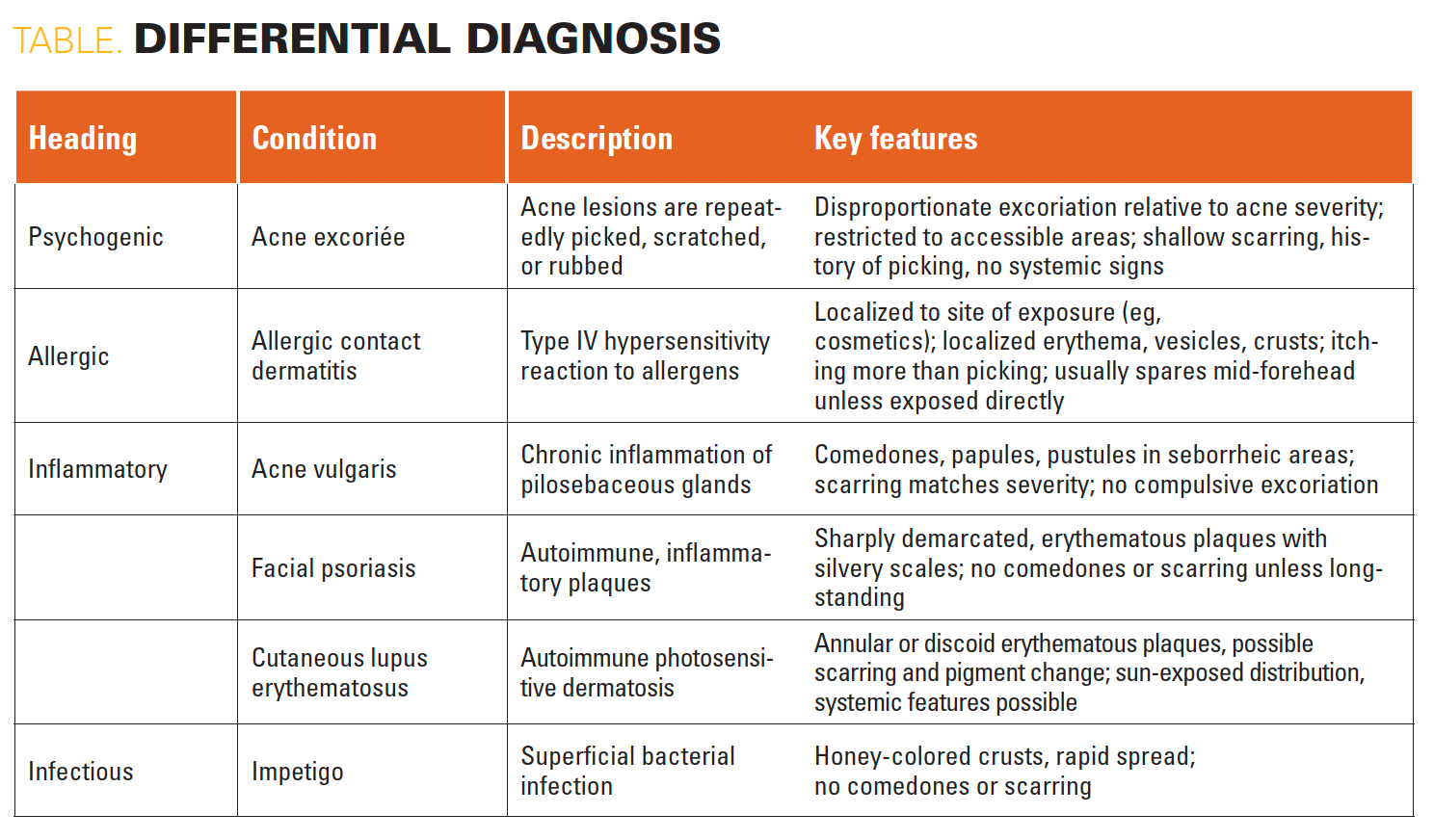
In addition, contact dermatitis presents with erythematous, vesicular, or crusted lesions in response to allergens or irritants (such as cosmetics or skin care products). Unlike acne excoriée, the primary symptom is pruritus rather than picking, and lesions are localized to the site of contact.8
Acne vulgaris, a more common inflammatory condition, presents with comedones, papules, and pustules in seborrheic areas. The scarring in acne vulgaris typically correlates with lesion severity and inflammation, and compulsive excoriation is not a defining feature.9
Facial psoriasis may also resemble acne excoriée, especially when lesions are excoriated. However, it is characterized by sharply demarcated erythematous plaques with silvery scale, often affecting the scalp, and lacks comedones or active acneiform lesions.10
Cutaneous lupus erythematosus is an autoimmune dermatosis that may present with erythematous annular plaques and pigmentary changes in sun-exposed areas, occasionally leading to scarring.11 Systemic symptoms or a photosensitive distribution can help differentiate it from acne excoriée.
Infectious causes such as impetigo must also be considered, especially in children and adolescents. Impetigo presents with characteristic honey-colored crusts, often around the nose and mouth, and can spread rapidly. The absence of comedones and a history of acute onset with bacterial exposure help distinguish it from psychogenic skin disorders.12
Management
Managing acne excoriée requires a multidisciplinary approach that addresses dermatological and psychological components. Numerous studies in recent years have emphasized the importance of combining pharmacologic treatment, behavioral therapy, and dermatologic interventions.13
The first step is to manage the underlying acne using standard therapies such as topical retinoids, benzoyl peroxide, and systemic antibiotics to reduce primary lesions and discourage picking.14 N-acetylcysteine, a glutamate modulator, has
also shown efficacy in reducing skin-picking behavior, particularly in patients with compulsive tendencies.15
Psychiatric comorbidities such as OCD, anxiety, and SPD must also be addressed. Pharmacologic treatment with selective serotonin reuptake inhibitors (eg, fluoxetine, escitalopram), serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants has shown effectiveness in managing these disorders.15
Behavioral interventions are crucial for long-term management. Cognitive behavioral therapy (CBT), habit reversal training, and other psychotherapeutic techniques have demonstrated lasting benefits in managing compulsive behaviors. Studies have also linked high impulsivity traits with acne excoriée, further justifying the need for psychological evaluation and tailored intervention.
Conclusion
Acne excoriée is a psychodermatologic condition requiring dermatological and psychological intervention. Early diagnosis, acne control, and behavioral therapies like CBT are key to preventing long-term scarring and distress. Prognosis varies—although many improve with a multidisciplinary approach, others may face persistent pigmentary changes and relapse without adequate support.
References
- Johnsen N, Poppens M, Cheng K. Acne excoriée: diagnostic overview and management. Int J Dermatol. 2024;63(5):565-571. doi:10.1111/ijd.16964
- Öğüt Ç, Öğüt ND. Impulsivity in patients with acne excoriee. J Cosmet Dermatol. 2023;22(3):1099-1104. doi:10.1111/jocd.15535
- Tavallaei AM, Sardabi MS, Ferezghi MR. Adolescent acne excorie: features and the use of cognitive behavioral therapy. In: Martin CR, Patel VB, Preedy VR, eds. Handbook of Lifespan Cognitive Behavioral Therapy. Academic Press; 2023:81-87.
- Georgescu SR, Sârbu MI, Mitran CI, Mitran MI, Benea V, Tampa M. Diagnostic challenges and treatment difficulties in a patient with excoriated acne conglobata. J Mind Med Sci. 2017;4(1):74-79. doi:10.22543/7674.41.P7479
- Oakley A. Acne excorie. DermNet. Updated April 2014. Accessed April 21, 2025. https://dermnetnz.org/topics/acne-excorie
- Kostner L, Anzengruber F, Guillod C, Recher M, Schmid-Grendelmeier P, Navarini AA. Allergic contact dermatitis. Immunol Allergy Clin North Am. 2017;37(1):141-152. doi:10.1016/j.iac.2016.08.014
- Oge' LK, Broussard A, Marshall MD. Acne vulgaris: diagnosis and treatment. Am Fam Physician. 2019;100(8):475-484.
- Bronckers IM, Paller AS, van Geel MJ, van de Kerkhof PC, Seyger MM. Psoriasis in children and adolescents: diagnosis, management and comorbidities. Paediatr Drugs. 2015;17(5):373-384. doi:10.1007/s40272-015-0137-1
- Elmgren J, Nyberg F. Clinical aspects of cutaneous lupus erythematosus. Front Med (Lausanne). 2023;9:984229. doi:10.3389/fmed.2022.984229
- Nardi NM, Schaefer TJ. Impetigo. In: StatPearls. StatPearls Publishing; July 31, 2023. Accessed October 15, 2025. https://pubmed.ncbi.nlm.nih.gov/28613693/
- Nemeh MN, Hogeling M. Pediatric skin picking disorder: a review of management. Pediatr Dermatol. 2022;39(3):363-368. doi:10.1111/pde.14953
- Leung AK, Barankin B, Lam JM, Leong KF, Hon KL. Dermatology: how to manage acne vulgaris. Drugs Context. 2021;10:2021-8-6. doi:10.7573/dic.2021-8-6
- Grant JE, Chamberlain SR, Redden SA, Leppink EW, Odlaug BL, Kim SW. N-Acetylcysteine in the treatment of excoriation disorder: a randomized clinical trial. JAMA Psychiatry. 2016;73(5):490-496. doi:10.1001/jamapsychiatry.2016.0060
- Mashayekhi Goyonlo V, Sardabi MS, Tavalaei AM, Khoshnevisan Z, Razmara M. Cognitive behavioral therapy as an adjuvant therapy in acne excoriée: a randomized controlled clinical trial. J Dermatolog Treat. 2022;33(2):782-788. doi:10.1080/09546634.2020.1776207
- Schumer MC, Bartley CA, Bloch MH. Systematic review of pharmacological and behavioral treatments for skin picking disorder. J Clin Psychopharmacol. 2016;36(2):147-152. doi:10.1097/JCP.0000000000000462
Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.