Tools for taming otitis media
The best devices for helping the 5 million children diagnosed with acute otitis media each year.
According to the American Academy for Pediatrics (AAP), there are over 5 million children diagnosed with acute otitis media (AOM) each year in this country.1 This results in 30 million visits for medical care and is responsible for over 10 million antibiotic prescriptions yearly.1-3 The increasing incidence of antibiotic resistance among the organisms responsible for AOM is a cause for concern. Although pneumococcal vaccine has reduced the incidence of AOM, by 1 year of age 23% of children have experienced one or more episodes of AOM and 3.6% have had 3 or more episodes.1 By 3 years of age, 60% of children have had one or more episodes of AOM and 24% have had 3 or more episodes.1 Otitis media with effusion (OME), or fluid behind the tympanic membrane without infection, often precedes or follows AOM. Although it does not require antibiotic treatment, persistent or recurrent OME can have significant impact on a child’s hearing and the structure of the middle ear space. The AAP recommendations, last updated in 2013, describe several criteria for diagnosing AOM and distinguishing this condition from OME.3 This article will describe how pediatricians can use various devices to assist in the diagnosis and monitoring of AOM as well as OME.
Guidelines for AOM and OME
The AAP issued extensive AOM guidelines in 2004 recommending that pediatricians make efforts to more accurately diagnose AOM and distinguish AOM from OME. They also developed criteria for treating children with antibiotics or monitoring symptoms when withholding antibiotics.2 Subsequent surveys of AAP members demonstrated that the 2004 guidelines did not change clinical practice, and so the AAP revised their AOM guidelines in 2013.3 The 2013 guidelines recommend that (1) the diagnosis of AOM should be made in a child with bulging of the tympanic membrane or otorrhea when otitis externa is excluded and (2) clinicians should diagnose AOM in children who present with mild bulging of the tympanic membrane and recent (less than 48 hours) onset of ear pain or intense erythema of the tympanic membrane. Most importantly, the guidelines state that, “The diagnosis is excluded if middle ear effusion is not present based on pneumatic otoscopy or tympanometry.”3
The reality of AOM diagnosis
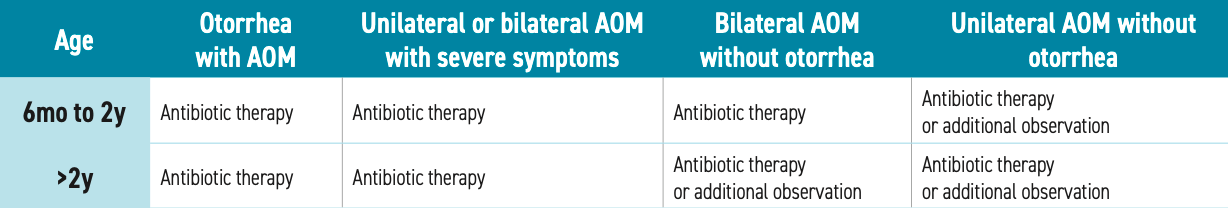
Despite evidence-based recommendations from the AAP, few pediatricians utilize pneumatic otoscopy and or tympanometry to diagnose otitis media. We should learn to utilize current technologies to exclude the diagnosis, or at least try to diagnose the condition with more certainty. There are many children with recurrent episodes of AOM who have hearing loss who become candidates for placement of tympanostomy tubes. Moreover, although previous recommendations suggested withholding antibiotics, the most recent guidelines are more liberal regarding when antibiotics should be used (see Table).3
Table
Visualizing the tympanic membrane
During their career, a pediatrician looks at thousands of ear canals and tympanic membranes, so presumably we’d would be pretty good at detecting bulging of the tympanic membrane and erythema. Truth be told, the diagnosis is often difficult. Early in the course of otitis media, there may be minimal bulging or slight erythema of the tympanic membrane. Additionally, a crying child will often have injection of the tympanic membrane which may be incorrectly interpreted as erythema.
Welch Allyn Macroview

Fortunately, we now have several new devices that help visualize the tympanic membrane and ear canal. It is likely you are currently using a Welch Allyn MacroView Otoscope to peer into your patients’ ears. This device provides a wider view and more illumination than its predecessor. Now Hillrom, who produces this otoscope, has improved upon the MacroView with the introduction of the MacroView Plus Otoscope.4 The MacroView Plus Otoscope provides up to 3 times the field of view than traditional otoscopes, and when it is used in conjunction with their new (and backward compatible) LumiView clear single use speculum, illumination is up to 8 times brighter than it is with their black speculum. They even have a new, slimmer, Lithium Ion Plus USB handle, which can be charged via a USB-C port, that retains a charge longer and is more ergonomic than previous models. In addition, the MacroView Plus can be attached to an Android phone or iPhone with their SmartBracket accessory. The SmartBracket places the camera lens of the phone over the viewing port of the otoscope. Using an application on the attached smartphone, one can capture (and enhance) the image of the tympanic membrane and transfer the image to a computer to include in the medical record or show to the parent and patient.4
I have long been a fan of the Wispr Digital Otoscope5 from WiscMed. The device is a digital video otoscope head that fits most traditional otoscope handles. It enables one to take a picture or video of the ear canal and tympanic membrane and display the image on a screen. One can transfer images via USB drive to a computer for inclusion in the medical record. Parents and patients are always impressed with the Wispr images, and it now includes a “pediatric” mode that displays cartoon characters that can be used to engage patients and help with cooperation.
Wispr

Is hearing affected?
Not only is it important to visualize the ear canal and tympanic membrane when a child presents with fever and ear pain, but it is also important in many circumstances to establish whether a child’s hearing is normal or not. Pediatricians can determine whether a child with recurrent or persistent otitis has a hearing loss with otoacoustic emissions (OAE) screeners that can rapidly determine if a child has a hearing loss and can quantify the hearing loss with pure tone audiometry. Given that OAE screeners generate a “pass or refer” result, pediatricians should consider performing a pure tone audiogram to determine the hearing threshold for the child. Be aware that 20% of children aged 3 to 5 years will not be able to be screened by pure tone audiometry, and those unable to be screened should be evaluated by an audiologist. Hearing screeners such as the Bio-logic AuDX Pro and AuDX Pro Flex6 from Natus Medical are modular devices that facilitate screening in the primary care office. The Bio-logic AuDX Pro can be configured to display a cartoon to distract a child during the brief OAE screen. Additionally, it can be used to perform pure tone audiometry on children who refer on OAE screen or for those suspected as having auditory neuropathy. The Bio-logic AuDX Pro Flex provides all the capabilities of the AuDX Pro as well as providing tympanometry capability. In the latter situation, 1 device provides all the hearing screening capability a practice requires.6
When fluid is present
As pediatricians do not uniformly perform pneumatic otoscopy, they can also perform tympanometry to determine whether fluid is present behind the tympanic membrane. Many OAE screeners include tympanometry as an add-on feature. Tympanometry requires a good seal between the probe tip and the ear canal and is difficult to perform in an uncooperative or crying child.
Many years ago, one of my favorite devices was the EarCheck Pro Middle Ear Monitor. The device directs sound at the tympanic membrane and records its reflection, determining a value called the spectral gradient angle (SGA). In seconds, without a seal, the device displays the SGA, which could indicate a middle ear effusion. The device was very popular in the 1990s, and there was also a home version so parents could monitor their children for effusions. Unfortunately, Becton Dickinson acquired the device, but never promoted it, and eventually production was halted. The device is going to reemerge either this year or early next year, as an acoustic otoscope7 from Check My EAR LLC. It will be able to assist pediatricians in assuring that an effusion is present in mere seconds, which is much faster than tympanometry.
Another device that can be helpful in diagnosing and monitoring AOM and OME is the OtoSight Middle Ear Scope8 from PhotoniCare. The device provides a true color video otoscopy of the ear canal and eardrum. Additionally, it determines the presence or absence of fluid in the middle ear; characterizes the type of fluid; and visualizes the fluid’s density, even in the presence of significant wax. The device is an optical coherence tomography otoscope that analyzes reflected light from the middle ear space to determine whether an infusion is present. Studies have shown that the device is very accurate in diagnosing OME.9 It is available via a monthly subscription.
OtoSight Middle Ear Scope

Another interesting device for diagnosing middle ear fluid is OtoNexus Medical Technologies’ Advanced Ultrasound Otoscope, which is reported to be unique in its ability to distinguish OME from AOM. The company has developed an inexpensive advanced otoscope that uses ultrasound technology to determine infection type with a high degree of accuracy. According to the company, this will enable clinicians to determine whether antibiotics are needed for treatment. The OtoNexus Ultrasound Otoscope10 is easy to use—pediatricians merely push a button when performing an otoscopic exam. The device displays a score that corresponds to both fluid presence and fluid type. FDA approval of the device is pending completion of clinical trials, and it is expected to be released sometime next year.10
Home otoscope
The COVID-19 pandemic has created an opportunity for the engineers at Remmie Health11 to develop and begin distribution of an inexpensive ($150) otoscope that can be used to capture images of the tympanic membranes and throat of an ill child or adult. The device is now available on Amazon and is designed to be nonthreatening to children. It complements ear or forehead thermometers that are likely used routinely by parents to screen children for fever. The Remmie Otoscope transmits images to a mobile application, allowing them to be sent to a child’s physician for review. As more and more physicians adopt telehealth, I anticipate that the Remmie Otoscope will prove useful for the otitis-prone child, as physicians can now diagnose otitis media or pharyngitis remotely. It can also be used to detect impacted cerumen and otitis external and to visualize foreign bodies in the ear canal.11
Conclusion
To provide optimal care for our patients, it is important to diagnose AOM accurately and distinguish it from OME. These technologies can help visualize the tympanic membrane; determine whether fluid is present in the middle ear space; and, most importantly, determine if the fluid is affecting a child’s hearing. By making these efforts, we can prescribe antibiotics more appropriately.
References
1. Kaur R, Morris M, Pichichero ME. Epidemiology of acute otitis media in the postpneumococcal conjugate vaccine era. Pediatrics. 2017;140(3):e20170181. doi:10.1542/peds.2017-0181
2. American Academy of Pediatrics; American Academy of Family Physicians. The diagnosis and management of acute otitis media. Pediatrics. 2004;113(5):1451-1465. doi:10.1542/peds.113.5.1451
3. Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e964-999.doi:10.1542/peds.2012-3488
4. MacroView Plus Otoscope. Accessed July 29, 2021. https://www.hillrom.com/en/products/macroview-plus-otoscope/
5. Wispr Digital Otoscope. Accessed July 29, 2021. https://www.wiscmed.com/wispr/
6. Biologic AuDx Pro Flex. Accessed July 29, 2021. https://hearing-balance.natus.com/en-us/products-services/bio-logic-audx-pro-flex
7. Acoustic Otoscope. Accessed July 29, 2021. https://www.affirmdx.com
8. OtoSight Middle Ear Scope. Accessed July 29, 2021. https://photoni.care
9. Preciado D, Nolan RM, Joshi R, et al. Otitis media middle ear effusion identification and characterization using an optical coherence tomography otoscope. Otolaryngol Head Neck Surg. 2020;162(3):367-374. doi:10.1177/0194599819900762
10. OtoNexus Medical Technologies. Accessed July 29, 2021. https://otonexus.com
11. Remmie. Accessed July 29, 2021. https://remmiehealth.com
Fluoxetine helps refractory nocturnal enuresis but not for long
March 29th 2023A 12-week study in Egypt of the efficacy of fluoxetine (a selective serotonin reuptake inhibitor) in children with treatment-refractory nocturnal enuresis (NE) found that though the treatment achieved a good initial response, it was not sustainable.
Meet the Board: Vivian P. Hernandez-Trujillo, MD, FAAP, FAAAAI, FACAAI
May 20th 2022Contemporary Pediatrics sat down with one of our newest editorial advisory board members: Vivian P. Hernandez-Trujillo, MD, FAAP, FAAAAI, FACAAI to discuss what led to her career in medicine and what she thinks the future holds for pediatrics.
Are some patients predisposed to avascular necrosis after hip surgery?
March 14th 2023Although avascular necrosis (AVN) is believed to be an iatrogenic complication following treatment of developmental dysplasia of the hip, an investigation in China found 2 characteristics associated with the condition: the likelihood of AVN increases with both the grade of dislocation and of underdevelopment of the ossific nucleus.
Meet the board: Jessica L. Peck, DNP, APRN, CPNP-PC, CNE, CNL, FAANP, FAAN
April 22nd 2022In the latest episode of our podcast series, Jessica L. Peck, DNP, APRN, CPNP-PC, CNE, CNL, FAANP, FAAN shares why she got into medicine, the myths of pediatric, and what the future may hold for the specialty.