Complications of Body Art
Henna and Hair DyeA 16-year-old Somali girl presented with a 30-day history of bilateral arm swelling and painful vesicular eruptions.Five days before presentation, she and her friends had used henna and black hair dye to “tattoo” their skin. Theothers did not experience similar signs or symptoms. This patient had used henna since childhood for decorativepurposes. However, outlining an intricate design with hair dye was new for her.This patient was hospitalized and treated for severe cosmetic dermatitis with systemic corticosteroids,diphenhydramine, and daily dry dressing changes. Ibuprofen was given to help relieve discomfort. Antibioticswere not ordered.The patient remained afebrile and was discharged on hospital day 2 with close follow-up and daily dressingchanges. She was advised to avoid contact with all hair-dye products.Case and photo courtesy of Jennifer A. Jewell, MD, and Lorraine L. McElwain, MD.

Henna and Hair Dye
A 16-year-old Somali girl presented with a 30-day history of bilateral arm swelling and painful vesicular eruptions.
Five days before presentation, she and her friends had used henna and black hair dye to “tattoo” their skin. The
others did not experience similar signs or symptoms. This patient had used henna since childhood for decorative
purposes. However, outlining an intricate design with hair dye was new for her.
This patient was hospitalized and treated for severe cosmetic dermatitis with systemic corticosteroids,
diphenhydramine, and daily dry dressing changes. Ibuprofen was given to help relieve discomfort. Antibiotics
were not ordered.
The patient remained afebrile and was discharged on hospital day 2 with close follow-up and daily dressing
changes. She was advised to avoid contact with all hair-dye products.
Case and photo courtesy of Jennifer A. Jewell, MD, and Lorraine L. McElwain, MD.
Tattooing and body piercing are popular among adolescents-many of whom may not be aware of possible medical complications. Tattooing is associated with transmission of hepatitis B and C viruses. Although transmission of HIV is theoretically possible, no instances have been definitively proved.Body piercing also has been implicated in the transmission of hepatitis.
In addition to infection, pain, bleeding, and allergic reactions-particularly to the pigments used in tattoos-keloids and scarring can occur (as illustrated in the following photos). Keloid response to skin injury is genetically determined; these scars occur more frequently in those with darkly pigmented skin and are associated with piercing.
Staphylococcus aureus, group A -hemolytic streptococci, and Pseudomonas species have been isolated from post-piercing infections. These have the potential to become life-threatening infections.
Risks specific to oral piercing include gingival recession, gum tissue injury, chipped and cracked teeth, excessive saliva production, and tongue swelling. Tongue or lip studs that unfasten can become choking hazards. Oral piercings can also result in altered speech and chewing problems.
7 THINGS YOU CAN DO
1 Advise your patient of the complications that are often associated with tattooing and piercing. Many persons who opt for body art are unaware of potential health risks and sequelae.
2 Describe the procedures of tattooing and body piercing to your patient. He or she may not know that tattooing involves multiple intradermal injections to achieve the design's color and pattern.
3 Emphasize the need for these practices to be performed in a sanitary environment by trained personnel (Table).
4 Stress the importance of appropriate wound care and aftercare. Prepare patients for the healing time needed after their procedure.
Mastitis After
Nipple Piercing
This red, indurated mass developed after the patient’s nipples had been pierced. The mass appeared almost 4 months after the piercing. It was painless, and had slowly enlarged. Fine-needle aspiration was performed; culture of the aspirate grew Mycobacterium fortuitum.
Case and photo courtesy of CPT Erin Drifmeyer, MD, and COL Ken Batts, DO.
The opinions and assertions contained herein are the private views of the authors and should not be construed as official or as reflecting the view of the Department of the Army or the Department of Defense.


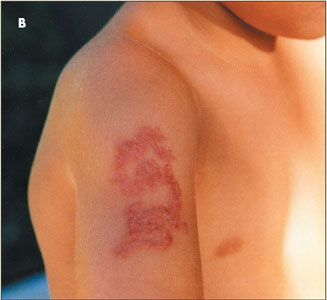
Henna Tattoos
The children in these pictures-a brother and sister-had received henna tattoos. The tattoo site became
pruritic 2 days after application in both siblings. Eleven days later, the color had faded but an exact outline of
the original tattoo remained. The lesions were papular, eczematous, erythematous, and extremely pruritic
(Figures A and B).
These children were treated with topical corticosteroids and oral antihistamines. The rash persisted in both
children 22 days after the henna had been applied. At day 30, the lesions were still evident in the form of a
hypopigmented macula that marked the outline of the original “art” (Figures C and D). These hypopigmented lesions may become permanent marks.
Case and photos courtesy of Angel Cadiz, MD.


5 Recommend the following care for new tattoos:
-Wash tattoos frequently with soap and water and apply antibiotic ointment for the first 2 to 3 days. Thereafter, keep the area clean and apply lotion to prevent drying and scabbing.
-Seek medical evaluation if skin redness or whitish drainage persists beyond the first few days.
-Do not rub or dislodge the scab that will form and remain for 1 to 2 weeks.
-Do not swim or use saunas or steam rooms until the area has healed.
-Apply sunblock to all exposed skin, including tattoos; sunlight fades the pigments.

Allergic Reaction to a Tattoo
After exposure to the sun, an erythematous, edematous, pruritic allergic reaction developed at the site of a new tattoo. In addition to photoallergy-as seen in this patient-direct allergy to the dyes in the tattoo can produce an adverse reaction.
This patient underwent carbon dioxide laser tattoo removal with good results.
Case and photo courtesy of Alan B. Schliftman, MD.
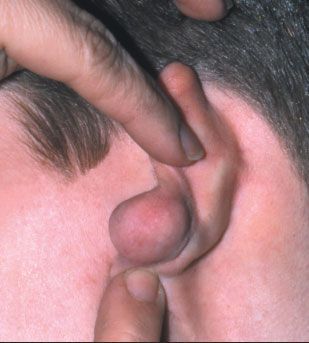
Bilateral Keloids Following
Ear Piercing
Postoperative inflammation occurred shortly after this patient’s earlobes were pierced. Within a few months, bilateral keloids developed. The keloid on the left ear is shown here. A 4-month course of intralesional triamcinolone acetonide injections (40 mg/mL once a month) was followed by carbon dioxide laser surgery to remove the keloid on the left ear. A postoperative intralesional injection of triamcinolone acetonide was given monthly for 6 months.
The keloid on the right ear was surgically excised after 4 months of triamcinolone acetonide injections.
The postoperative regimen was identical to that of the left ear. The surgically excised keloid recurred within 4 months; the laser-treated left ear remained free of the scarring 2 years longer than the right ear.
Case and photo courtesy of Alan B. Schliftman, MD.
6 Emphasize the following care for piercings:
-Select high-quality jewelry, such as rings and ornaments made from surgical steel, 14-carat gold, niobium, or titanium. Do not use jewelry made of nickel; a contact dermatitis can develop.
-Apply ice for swelling, if necessary.
--Do not allow pierced areas to come in contact with unclear hair, hands, clothing, or bed linens.
-Wash the area with antibacterial soap twice daily; rinse well; rotate jewelry; and dry the area thoroughly.
-Use antiseptic ointment for 1 week only; after eating, rinse oral piercings with mouthwash that does not contain alcohol.
-Do not use alcohol, hydrogen peroxide, or iodine on the wound.
-Avoid public pools, hot tubs, spas, and the body fluids of others until the pierced area is completely healed.
-Expect redness and slight discharge for a few days. Seek medical evaluation if oozing pus, swelling, or crusting develops.
7 Educate your patient about tattoo removal procedures. Explain that today's fashion statement may be passe tomorrow and while laser surgery, dermabrasion, or excision can be tried, these modalities can be risky and may not be completely successful. *


Scarring After Tattoo Removal
Three carbon dioxide laser treatments were used to remove this tattoo. Four
months after the procedures, significant scarring was noted at the site.
Case and photos courtesy of Alan B. Schliftman, MD.
References:
REFERENCE:
1.
Mayers LB, Judelson DA, Moriarty BW, Rundell KW. Prevalence of body art (body piercing and tattooing in university undergraduates and incidence of medical complications.
Mayo Clin Proc.
2002;77:29-34.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.