Elevated CPK: No short cut to muscular dystrophy diagnosis
A pediatrician with special training in neuromuscular disorders cautions that nothing replaces the traditional workup-a complete history and physical-for diagnosing neuromuscular complaints.
As medicine becomes more and more complicated, doctors are taking shortcuts that can profoundly hurt their patients. Taking histories, doing a complete physical examination, and talking with patients remain essential to good patient care. Instead, some doctors rush to order a battery of laboratory or genetic tests to replace a traditional workup.

Using an elevated creatine phosphokinase (CPK) as a standalone test for the diagnosis of muscular dystrophy (MD) can be a serious error and could have devastating consequences for patients. Ordering lab work may save time, but it is important for physicians to recognize the fallibility of the tests. Accurate interpretation of the studies requires the knowledge obtained from a complete history and physical (Table 1).
More: Pediatric high-grade glioma is not one tumor type but many
Two girls, ages 3 and 4 years, were seen in emergency departments (EDs) by doctors in different states with the complaint of “stomach ache.” Lab work was ordered, and both children showed markedly elevated CPKs. The mothers were told their daughters probably had Duchenne or Becker MD. The mothers consulted me. After reviewing the children’s medical records, I referred them to neuromuscular specialists. Both children were later found not to have the disease. A complete history and physical would have given the ED physicians the information they needed to avoid such a dire misdiagnosis. The parents suffered unnecessary fear for their daughters’ health and life. Both children were without any family history of MD and without the physical signs of the disease. The misdiagnosis was based solely on the elevated CPKs.
Possible reasons for elevated CPK
There are many possible explanations for an elevated CPK that must be considered prior to giving a child the death sentence of the diagnosis of Duchenne MD. First among these is a marked elevation that can be seen when blood is drawn from an active screaming child. (Elevated CPKs can also be seen in infants born after a high-risk delivery.1) They soon return to normal values. Other disorders associated with high CPKs are myositis and some types of myopathy. These conditions can have good outcomes if treatment is started early.
Myositis
Myositis can occur in several different forms. Viral myositis with weakness and an elevated CPK may develop after a respiratory infection and especially during a flu epidemic. The children develop mild muscle weakness and pain in their lower extremities that can keep them from wanting to walk. The symptoms improve after a few days. No treatment is required other than bed rest and careful monitoring.
Infantile myositis is frequently misdiagnosed as congenital MD.2 Only a few cases of infantile myositis have been reported in the literature.
NEXT: More MD cases
A girl was born at term after a normal pregnancy and delivery. At age 6 months, she was noted to have an elevated CPK of 2500 U/L and some mild hypotonia. A neurologist reported an electromyogram (EMG) to be myopathic. The muscle biopsy was signed out as congenital MD. On examination, I found the child to be extremely bright with just mild muscle weakness. A review of the muscle biopsy slides revealed none of the distinctive changes of congenital muscular dystrophy.
I had the original block recut and stained. Three of the 11 sections showed a striking perivascular inflammatory response. After a 2-week course of prednisone (1 mg/kg), the patient showed increased muscle strength and tone. After 3 months, the CPK was within normal limits. The child continued to improve and soon was able to take a few steps in long-leg braces. I have a long-term follow-up of the child. Although she has needed intermittent steroids, she has done well.
Polymyositis
Polymyositis is too often diagnosed as Duchenne MD. This is a treatable condition with excellent results when the diagnosis is made and prednisone treatment started in the early phases.
Recommended: 7 lower limb positional variations
Doctors John Walton (Lord Walton) and Raymond Adams wrote the definitive text about polymyositis in 1958.3 I was fortunate to spend time in Dr. Walton’s neuromuscular unit at the University of Newcastle located in Newcastle upon Tyne, United Kingdom, when he was dean of the medical school there. His teaching has allowed me to diagnose many cases of this disorder. It is exciting to watch patients respond to treatment once steroids are started. Initially, steroids should be given in a large dose (1 mg/kg-2 mg/kg) and then tapered off as the CPK lowers and the patient’s muscle strength improves.
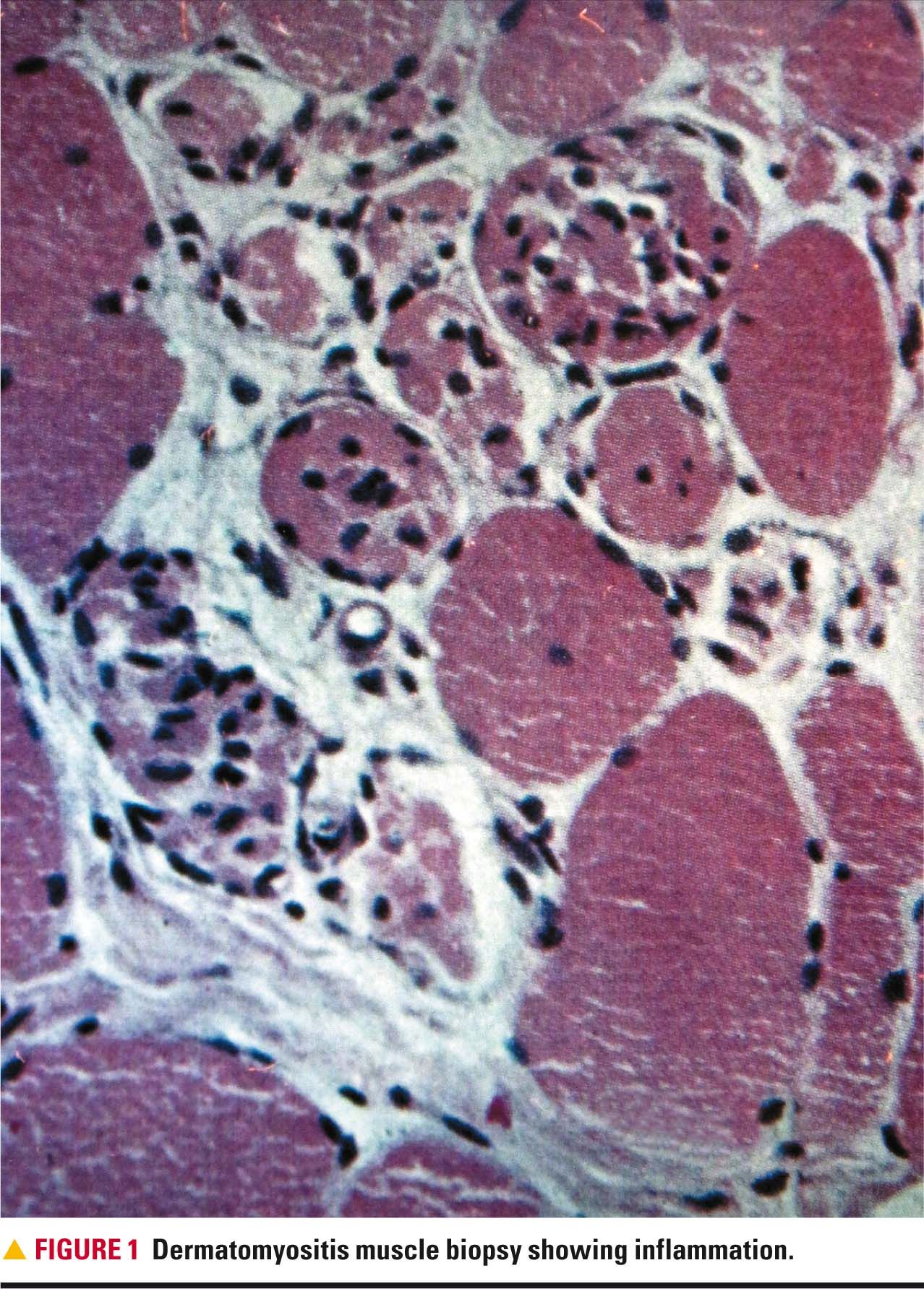
Dermatomyositis
Another form of myositis is dermatomyositis (Figure 1).4 When these patients are seen by orthopedists or neurologists, they are frequently diagnosed as having some type of MD. If a pediatrician has a patient with muscle weakness and any kind of a skin rash, I would want the child or teenager to be immediately referred to a rheumatologist or a neuromuscular specialist who treats dermatomyositis.

A 16-year-old girl complained of increasing muscle weakness. On examination, I found her to have mild proximal weakness, skin lesions typical of dermatomyositis, and a CPK of 1552 U/L. A muscle biopsy was done using a local anesthetic. The slides revealed typical inflammatory cells and other features of myositis. A daily initial dose of 60 mg of prednisone brought remarkable results. She slowly improved allowing the prednisone to be reduced. Her recovery was complete after many months of treatment. She later married and now dances with her husband’s band (Figure 2).

A 5-year-old boy saw an orthopedic surgeon because of mild muscle weakness. The physician, on the basis of an elevated CPK and Gower sign (indicating hip girdle weakness), told the parents their son had Duchenne MD. When I saw the child for a neuromuscular workup, he had skin lesions typical of dermatomyositis. A muscle biopsy was performed using a local anesthetic and showed multiple inflammatory cells. The boy responded remarkably well to prednisone and we kept in touch for many years. He became a music instructor at a university.
NEXT: Emery-Dreifuss muscular dystrophy
A neurologist in a university medical school saw a 4-year-old girl because of her slowly increasing proximal muscle weakness. She also showed weakness of the neck muscles. Her parents reported weight loss and difficulty swallowing. A CPK of 4700 U/L was reported. A muscle biopsy showed a myopathy with no specific diagnosis. The neurologist told the parents the diagnosis was most likely MD because of the elevated CPK.
The parents did some research and remembered that their daughter had had a rash several months before. They had been referred to a dermatologist and cortisone was prescribed with some improvement of the rash. The mother brought her daughter to see me, and on examining the child, I found diffuse proximal weakness of the pelvic and shoulder muscles. She also had a positive Gower sign upon trying to get up from the floor and marked neck weakness. I did not see any rash at that time.
More: Does strep elevate risk of mental disorders?
On reviewing the muscle biopsy, I saw diffuse inflammation and some areas of focal inflammation. There were also some nonspecific changes. I diagnosed dermatomyositis and started the child on prednisone 1 mg/kg. The family returned to their home and I worked with their pediatrician to be sure the child received an adequate dose of prednisone. The mother and I kept in contact by telephone and e-mail. The little girl did well. Two years ago, I received a lengthy e-mail bringing me up to date. The mother said the girl was now a healthy 20-year-old.
Signal recognition particle myopathy
Signal recognition particle (SRP) myopathy is a fairly newly described disorder that mimics polymyositis.5 It can also be mistaken for MD.
A teenager who excelled in sports began to lose muscle strength, so his parents consulted a neurologist at a major university medical center. The physician diagnosed limb-girdle MD and scheduled the boy for over 200 genetic tests. When the family contacted me, the adolescent’s history indicated a myopathy, possibly myositis. Patients who have limb-girdle MD don’t suddenly become weak after being good athletes. I referred him to the Mayo Clinic, and the workup there revealed SRP. His initial CPK there was 11,000 U/L. The boy responded well to prednisone and methotrexate and is active in sports once again.
Emery-Dreifuss muscular dystrophy
Emery-Dreifuss MD is an unusual muscle disorder. It is important to diagnose this disease correctly because it can cause sudden death in teenagers or adults from cardiac involvement. Insertion of a pacemaker can be lifesaving. This is a sex-linked recessive disorder, so mothers also may be at risk for cardiac problems and might need a pacemaker.
A 10-year-old boy had been given the diagnosis of MD because of a CPK of 656 U/L and some muscle weakness. When I first examined the child, his physical exam revealed mild muscle weakness, but not in a typical pattern for Duchenne MD. A muscle biopsy, done using a local anesthetic, showed some unusual muscle cells, but no characteristics of Duchenne MD. I told the child’s mother that no definite diagnosis could be made at that time and suggested that we wait to see if any progression occurred. I followed the boy at regular intervals. He showed no increased weakness.
Five years later, I attended a lecture by Dr. Lewis Rowland from Columbia University, New York. He presented 5 cases of a newly described disorder called Emery-Dreifuss MD.6 The symptoms and muscle biopsy were similar to my patient’s. Dr. Rowland reviewed my patient’s muscle biopsy slides and record. He confirmed it was a classic case of Emery-Dreifuss MD. The disorder can cause a severe arrhythmia that requires a pacemaker. My patient’s mother also was a candidate for a pacemaker. The boy had a pacemaker inserted as a teenager and his mother had the procedure in her early fifties. My patient died at age 52 years from cardiac problems but his mother is still living.
NEXT: Duchenne muscular dystrophy
Duchenne muscular dystrophy
Duchenne MD is a sex-linked disorder, and two-thirds of the cases are genetic. The disorder has very specific diagnostic signs. The CPK can be extremely high, sometimes in the many thousands. Boys are generally late walkers and even small boys show beginning proximal weakness, tightness of the heel cords, and difficulty getting up from the floor (Gower sign). As the disease progresses, the heel cord tightness causes the boys to walk on their toes.
Stretching of contractures and heel cord lengthening done at the proper time can greatly improve boys’ ability to get around. Contractures develop in a very specific pattern. Two-thirds of the patients show some developmental delay and learning disabilities. Calf enlargement also may be present.
Prednisone treatment is still advocated by Victor Dubowitz, MD, Professor Emeritus of the Royal College of Paediatrics and Child Health, London, United Kingdom (personal communication, 2016). He is a pediatric neuromuscular specialist and founder of the World Muscle Society. Now new drugs are also being tried.
The muscle biopsy is very specific. Scoliosis and cardiac and pulmonary problems develop as the boys age. Keeping them ambulatory and watching for increased weight gain and blood pressure are extremely important.
Becker muscular dystrophy
Becker MD is another sex-linked recessive disorder. It is much more benign than Duchenne MD and usually has a later onset. The CPK can be markedly elevated. Boys may develop mild muscle weakness and can have difficulty being as active as friends their own age. Walking can be possible until the early 30s. Mild contractures may develop and the calves may be enlarged. Cardiac problems are important to watch for, and the mothers who are carriers may also develop cardiac difficulties.
Malignant hyperthermia (MH) is associated with MD.7 Patients with both Duchenne MD and central core disease are at risk. The gene for this disorder, 19q, and the gene for central core disease are the same, so these patients are at particular risk. Malignant hyperthermia can cause severe problems during a surgery and even death if the anesthesiologist is not prepared to treat the problems that can develop.
When a child has muscle weakness, it is important to ask if a relative has ever had problems with an anesthetic. The drug sevoflurane and its related agents should not be used. Also, the anesthetic machine should be flushed out prior to any surgery on a patient with muscle weakness. If a child manifests this disorder, other family members should be alerted as they, too, may be at risk. There is an MH hotline with an anesthesiologist always available to answer calls: 1-800-644-4917.
Next: Two potential drugs to treat Dravet syndrome
A complete neuromuscular workup must be done before any diagnosis of a muscle disorder is made (Table 2). A neuromuscular workup includes the patient’s history; a family history of muscle weakness or anesthetic problems; and a complete physical examination with the patient undressed down to his/her shorts or underpants. A muscle biopsy is performed using a local anesthetic because of the risk of MH. A CPK lab test, and genetic tests if indicated, complete the workup. Until all these are done, no diagnosis of a muscle disease should ever be made.
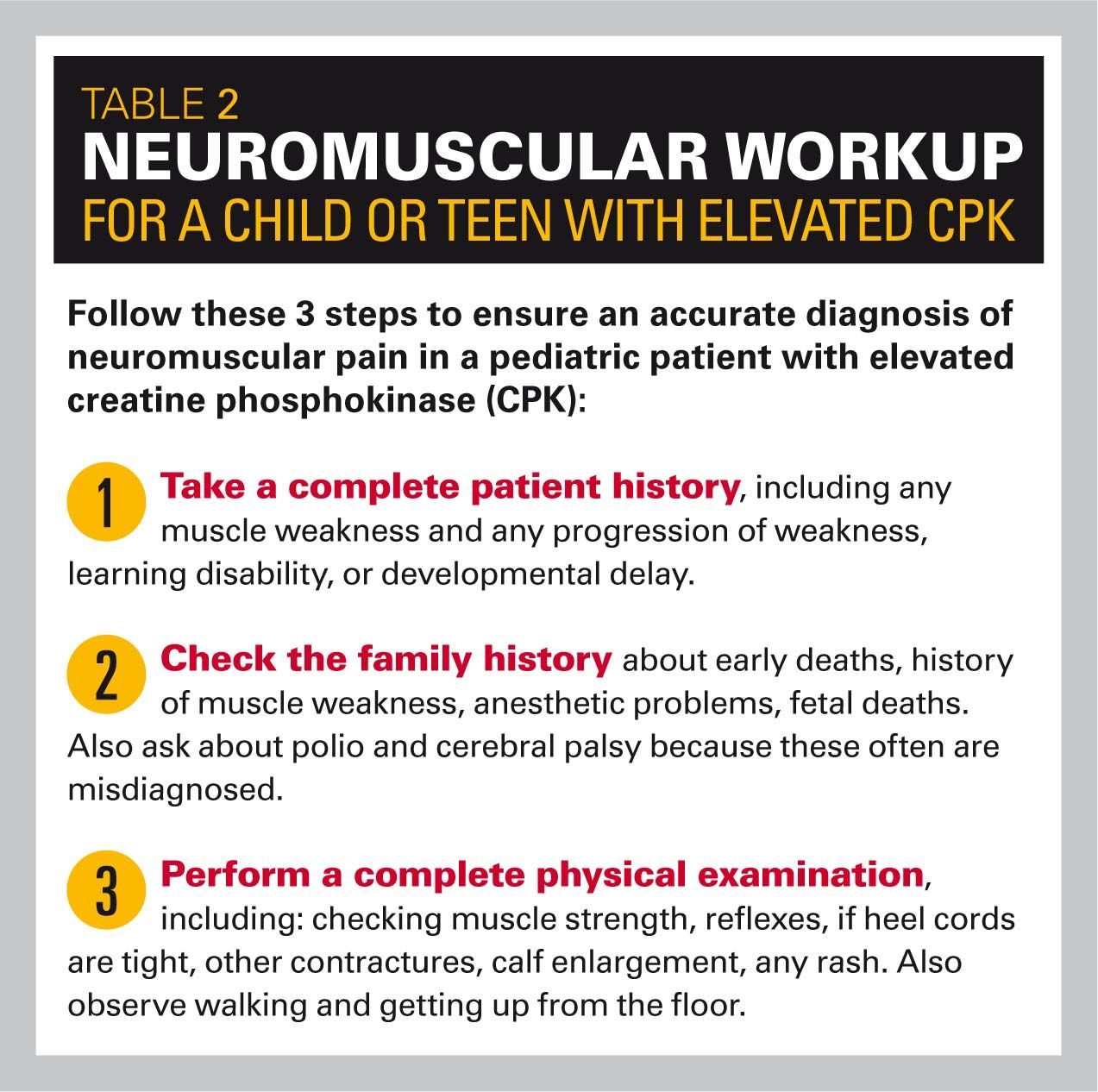
Experts say a muscle biopsy can guide a physician to order the appropriate gene studies. I am told by Caroline Sewry, professor of Muscle Pathology at Dubowitz Neuromuscular Centre, London, England, that gene studies do not always pick up deletions and duplications (personal communication, 2017).
If the diagnosis of a muscle disorder is confirmed, communication with the parents should always be done face-to-face, not over the telephone. Parents hear the words ”muscular dystrophy” and their world topples.
In summary
Making the diagnosis of Duchenne or Becker MD on the basis of a single elevated CPK can be a tragic error resulting in fear and pain for the parents. The 8 cases I presented here show the fallibility of doing this. Myositis in different forms can have markedly elevated CPKs, but the CPK can be normal in about 25% of cases. Early treatment with prednisone and sometimes additional drugs can completely reverse the muscle weakness.
Emery-Dreifuss MD patients can have a moderate elevation of CPK. This diagnosis is important to make because the insertion of a pacemaker for arrhythmia can be lifesaving. Limb-girdle MD patients may have a moderately elevated CPK and a much longer life span than Duchenne patients.
The importance of a complete workup for a muscle disease is imperative before parents can be given a specific diagnosis.
REFERENCES
1. Cuestas RA Jr. Creatine kinase isoenzymes in high-risk infants. Pediatr Res. 1980;14(8):935-938.
2. Thompson CE. Infantile myositis. Dev Med Child Neurol. 1982;24(3):307-313.
3. Walton JN, Adams RD. Polymyositis. Baltimore: Williams and Wilkins; 1958.
4. Goebel H, Sewry C, Weller R. Muscle Disease: Pathology and Genetics. 2nd ed. New Jersey: Wiley-Blackwell; 2013.
5. Wang L, Liu L, Hao H, et al. Myopathy with anti-signal recognition particle antibodies: clinical and histopathological features in Chinese patients. Neuromuscul Disord. 2014;24(4):335-341.
6. Emery AE, Dreifuss FE. Unusual type of benign X-linked muscular dystrophy. J Neurol Neurosurg Psychiatry. 1966;29(4):338-342.
7. Thompson C. Raising a Child with a Neuromuscular Disorder. New York: Oxford University Press; 1999.
Dr Thompson is assistant clinical professor of Pediatrics, University of California San Diego School of Medicine, and the author of Raising a Child with a Neuromuscular Disorder (Oxford University Press; 1999). She has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.