Suspicious fever of unknown origin
A 5-month-old Hispanic boy, previously healthy, presents to the emergency department (ED) for 5 days of fever, 3 days of diarrhea and rash, and 2 days of vomiting. He had been diagnosed with acute otitis media by his primary care physician 3 days prior to his presentation and started on amoxicillin. The parents brought their son to the ED because of his persistent fever up to 104°F and decreased oral intake. He has no recent travel and no known sick contacts. His immunizations are up to date and he has never been hospitalized. He was born in the United States, full term with an uncomplicated birth history.
THE CASE
A 5-month-old Hispanic boy, previously healthy, presents to the emergency department (ED) for 5 days of fever, 3 days of diarrhea and rash, and 2 days of vomiting. He had been diagnosed with acute otitis media by his primary care physician 3 days prior to his presentation and started on amoxicillin. The parents brought their son to the ED because of his persistent fever up to 104°F and decreased oral intake. He has no recent travel and no known sick contacts. His immunizations are up to date and he has never been hospitalized. He was born in the United States, full term with an uncomplicated birth history.
Physical examination
On presentation to the ED, the patient is febrile to 103.5°F and tachycardic to 205 beats/minute, with blood pressure of 110/73 mm Hg while crying. Respiratory rate is 39 breaths/minute and his oxygen saturation is 99% on room air. He weighs 6.8 kilograms (13th percentile).
Physical examination reveals a fussy but easily consolable infant with soft and flat anterior fontanelle and II/VI systolic ejection murmur at the left upper sternal border. Lungs are clear with normal work of breathing. He has periorbital erythema with clear sclera, and moist lips and tongue. A blanchable, macular, erythematous rash on his trunk and groin is noted. The patient is uncircumcised with foreskin easily retracted. The rest of physical examination findings are unremarkable including bilateral ear examination.
Laboratory
Urinalysis, obtained by catheter, shows pyuria (10-20 white blood cells [WBC]), small leukocyte esterase, negative nitrite, and small ketones. Stool panel by polymerase chain reaction (PCR) is obtained and is positive for enterotoxigenic Escherichia coli (ETEC). Complete blood cell count (CBC) reveals mild leukocytosis with WBC of 11.9 x 103/mm3 (4-12 x 103/mm3), with 55% segmented neutrophils and 37% lymphocytes; platelets at 484,000 x 103/mm3 (140-440 x 103/mm3); hemoglobin, 8.5 g/dL (10.5-14 g/dL); hematocrit, 26.2% (32%-42 %) with mean corpuscular volume (MCV) at 59 fL (72-88 fL) and red cell distribution width (RDW) of 17.6% (11.5%-14.5 %). Electrolytes are: sodium (Na), 133 mmol/L (132-140 mmol/l); bicarbonate, 17 mmol/L (20-28 mmol/L); blood urea nitrogen (BUN), 8 mg/dL (10-18 mg/dL); creatinine, 0.3 mg/dL (0.2-0.5 mg/dL); and low albumin, 2.9 g/dL (4-5 g/dL). Blood and urine were sent for cultures and patient received a dose of 50 mg/kg intravenous (IV) ceftriaxone.
Hospital course
The patient was admitted to the general pediatric unit with presumed diagnosis of febrile urinary tract infection (UTI), acute bacterial gastroenteritis (ETEC), iron deficiency anemia, and viral exanthem (vs allergic reaction to amoxicillin). Ceftriaxone was continued for the presumed UTI. A renal ultrasound was obtained and revealed normal kidney size and echogenicity.
Eight hours into admission, the patient had decreased responsiveness and concern for altered mental status with a temperature of 105.3°F. lumbar puncture (LP) was completed and cerebrospinal fluid (CSF) showed mild pleocytosis with WBC of 14/mm3 (58% monocytes, 39% lymphocytes); red blood cell (RBC) of 25/mm3; glucose, 68 mg/dL; and protein, 15.4 mg/dL. Gram stain was negative. Empiric ceftriaxone dose was increased to cover for bacterial meningitis (100 mg/kg/d).
More: Pallor and swelling in an athlete's upper arm
Metabolic acidosis resolved with fluids. An iron panel supported the diagnosis of iron deficiency anemia, for which iron was prescribed. The patient’s emesis and diarrhea resolved, and his skin rash faded. Because all cultures were negative at 48 hours, ceftriaxone was discontinued, and the patient was thought to have aseptic meningitis as the source of his persistence fever. Cerebrospinal fluid enterovirus by polymerase chain reaction (PCR) assay was negative. Respiratory viral panel by PCR was obtained to test for other viral etiologies that could help explain the prolonged fever, but ultimately it was negative.
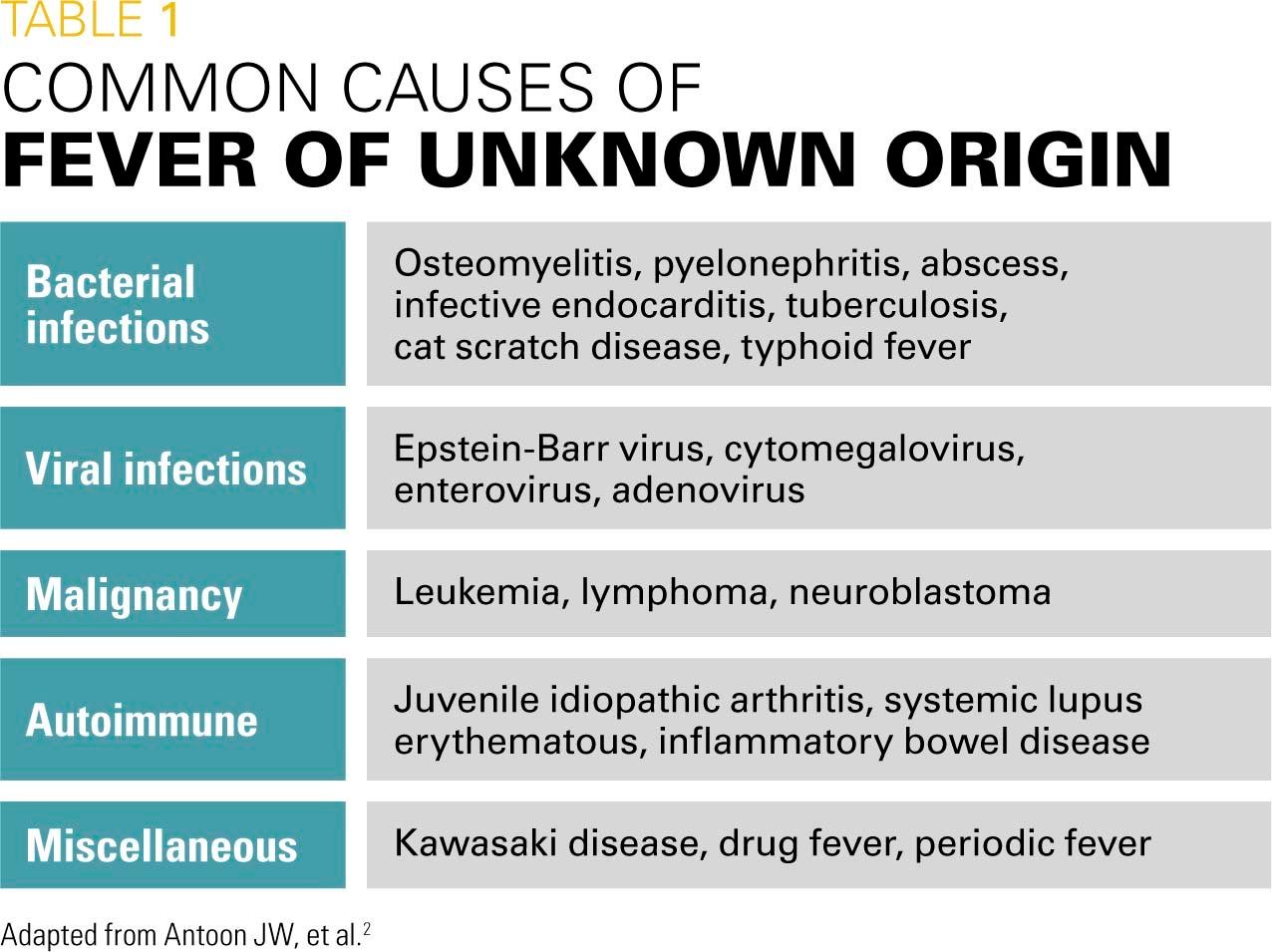
As the patient continued to have fevers without a source for more than 7 days, he met the definition of fever of unknown origin (FUO). The differential diagnosis of FUO is broad and includes infectious and noninfectious causes. See Table 1 for the most common causes of FUO.
Given the patient’s lack of clinical improvement, persistent unexplained fever greater than 102.2°F (mean maximal temperature [Tmax], 105.3°F), sterile pyuria, low albumin, mild thrombocytosis, neutrophil-predominant leukocytosis, CSF pleocytosis with negative culture, and significant sequelae of untreated Kawasaki disease (KD), inflammatory laboratories were drawn and resulted with elevated erythrocyte sedimentation rate (ESR) of 62 mm/h (0-13 mm/h) and C-reactive protein (CRP) of 8 g/dL (<0.3 g/dL). A repeat CBC revealed WBC of 16 x103/mm3 with 76% neutrophils, hemoglobin of 6.9 g/dL, and platelets of 486 x103/mm3. Repeat albumin was 2.4 g/dL.
NEXT: Discussion
Discussion
Fever, defined as a core body temperature equal to or greater than 100.4°F, is one of the most common complaints that brings a child to medical attention. The most common cause of a febrile illness in a well-appearing child is usually a self-limited viral infection.1 Once a fever without a clear source lasts more than a week, it becomes FUO by definition.2
Kawasaki disease is an acute childhood multisystemic vasculitis that can present as FUO. It is the main cause of acquired heart disease in Western countries in comparison with rheumatic heart disease in developing countries.3,4,5,6 If left untreated, KD can lead to devastating cardiac outcomes, as coronary artery aneurysms (CAAs) were reported in up to 25% of untreated patients.3,5,6 This number decreased to less than 5% after intravenous immunoglobulin (IVIG) was added to the treatment protocol.3,5 With the IVIG treatment window of 10 days or less since fever onset, one can see the importance of early recognition and treatment in avoiding cardiac complications.
The exact etiology of KD remains largely unknown, but one hypothesis suggests an infectious trigger in genetically susceptible individuals.4,7 Infectious trigger, likely viral, was suggested because of the seasonal peaks of the illness (winter and early spring in North America) and concomitant viral infections in many KD patients. Genetics plays an important role as KD is more common in children of Asian descent, particularly Japanese children in whom the annual incidence was 265 per 100,000 children aged younger than 5 years in 2012 compared with 25 per 100,000 children aged younger than 5 years in the United States.3,4
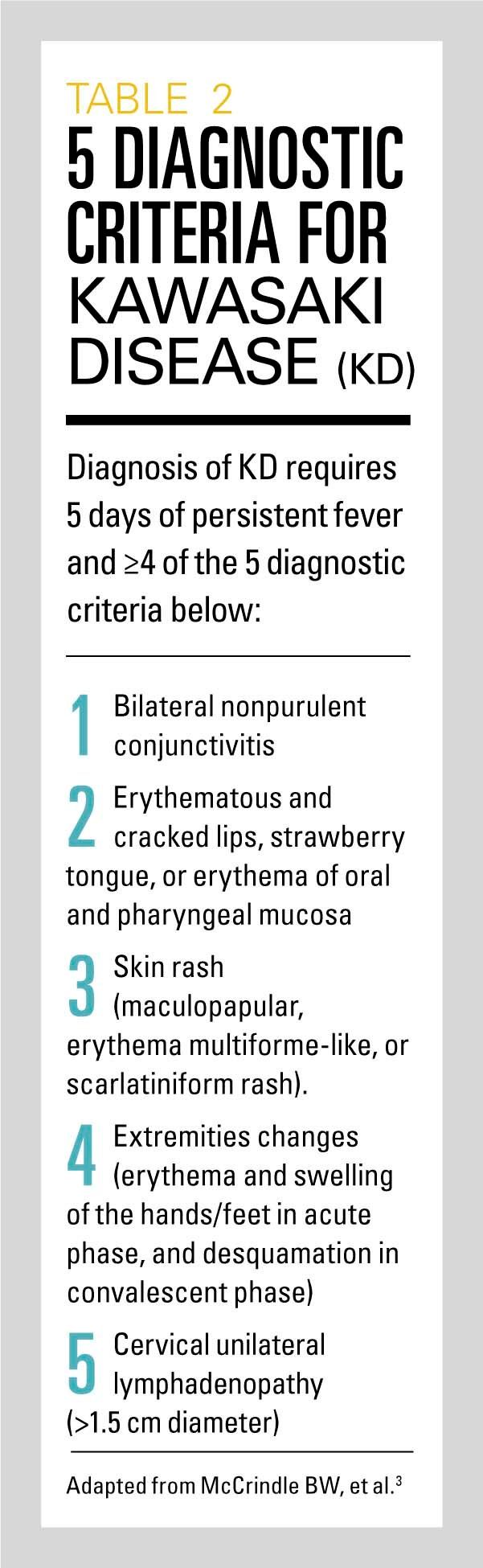
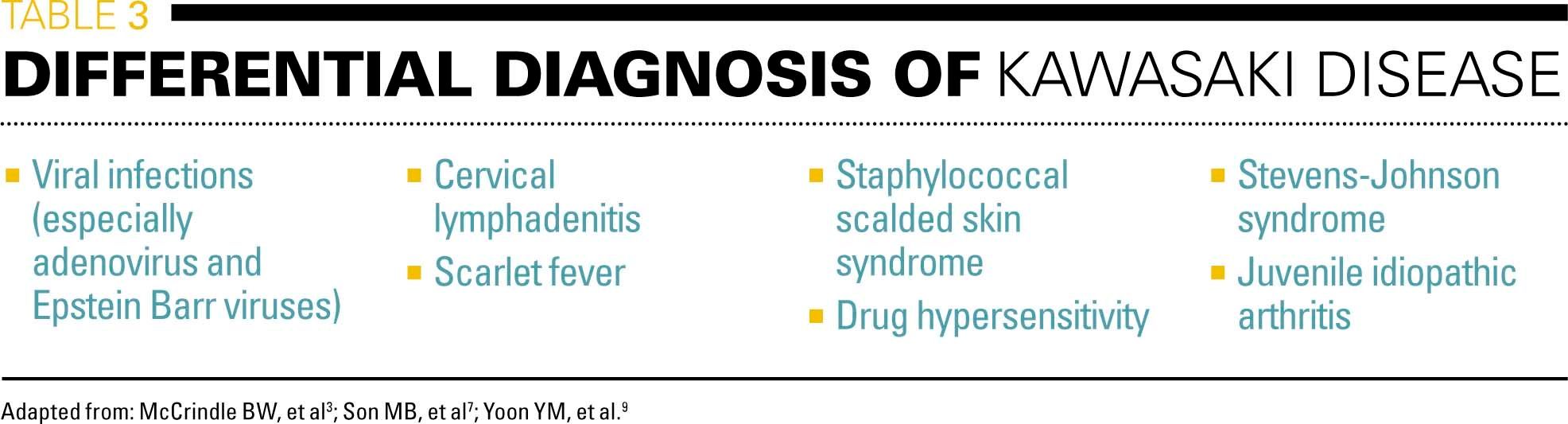
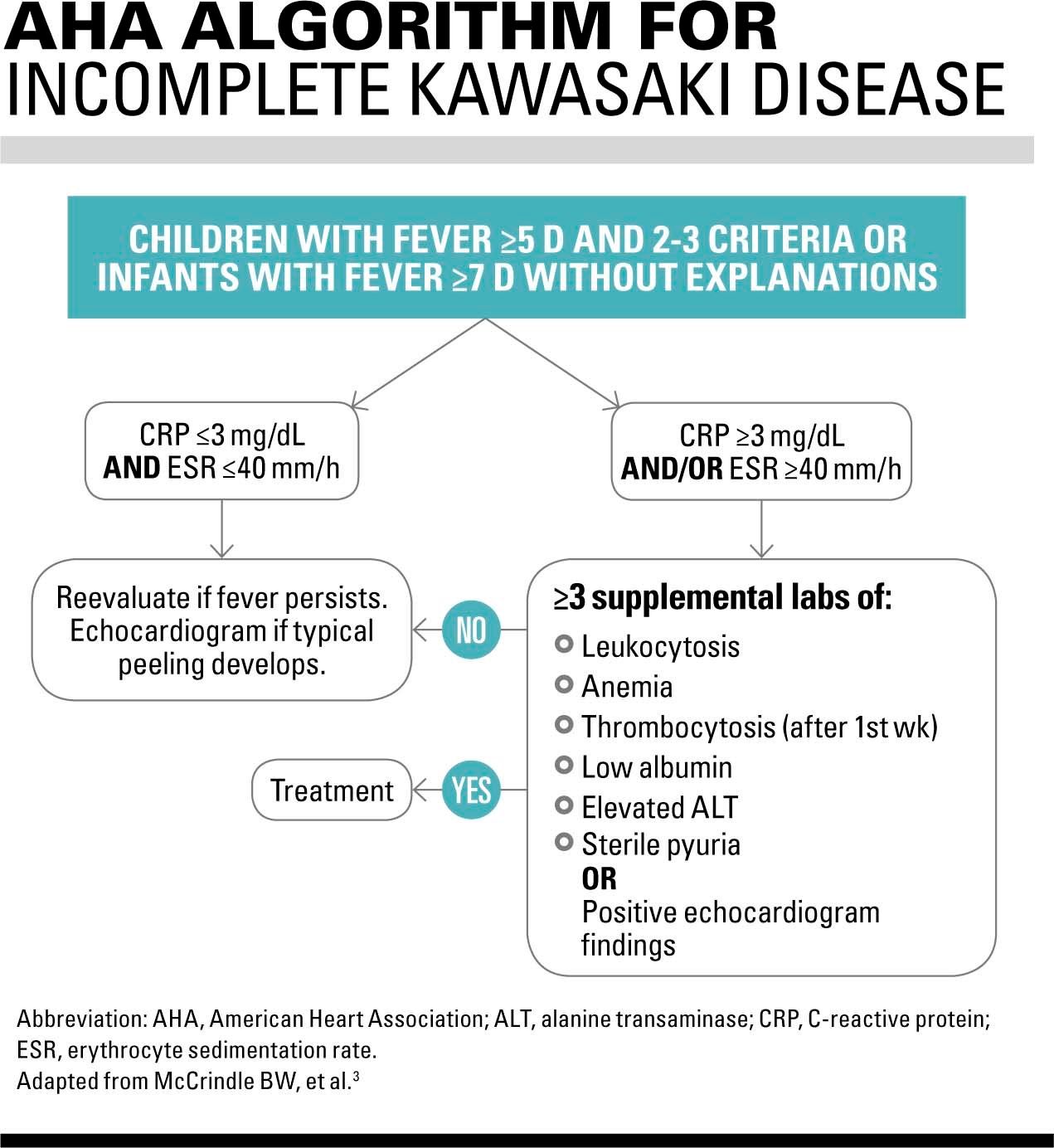
First described by Japanese pediatrician Dr. Tomisaku Kawasaki in 1967,6,8 KD has been traditionally classified as typical and atypical or incomplete disease. The diagnosis of typical, or complete, KD requires 5 days of persistent fever and 4 or more of the 5 diagnostic criteria shown in Table 2. It is important to note that these signs and symptoms can happen in sequence and not necessarily at the same time as presentation.4,5 Patients who have 5 days of fever and only 2 to 3 of these principal criteria can then be evaluated further according to the American Heart Association (AHA) algorithm (shown in Figure) for incomplete disease. The term “incomplete” is preferable to “atypical” as incomplete KD has similar clinical course to complete disease and nothing atypical is present other than fewer principal clinical features at presentation.7 Infectious causes, specifically viral, are among the main differential diagnoses of KD (Table 3).
KD in infants aged younger than 6 months
Kawasaki disease is a childhood vasculitis with 50% of cases occurring between ages 6 months and 2 years.5,9 The disease in infants aged younger than 6 months includes approximately 10% of all cases,5 and this age group is at higher risk for delayed diagnosis and coronary artery abnormalities.3,5,6,9 The nonspecific clinical features and absence of specific tests make it difficult to diagnose KD in general, and it is even more challenging in these infants because infantile KD can present with prolonged fever and irritability with no other clinical signs and symptoms (ie, no cervical lymphadenopathy, no conjunctivitis, and no hands or feet edema).3,6,7 Subsequently, maintaining a high index of suspicion in infants aged younger than 6 months with persistent unexplained fever is the key for diagnosis and timely treatment.
Related: Coronary artery lesions in Kawasaki disease are related to gene polymorphisms
The recent AHA guidelines recommend that infants aged younger than 6 months with 7 or more days of fever even without any other clinical manifestations should undergo laboratory investigation for incomplete KD.3
As was seen in this patient, KD in infants aged younger than 6 months can be misdiagnosed as febrile UTI or aseptic meningitis due to pyuria and pleocytosis, respectively, which might lead to delayed diagnosis and late treatment.
NEXT: Treatment of KD
Treatment of KD
High dose IVIG (2 g/kg/d) remains the cornerstone in treating KD, and although IVIG treatment decreases the risk of CCAs from 25% to 5%,3,5,6,7 there is no evidence that acetylsalicylic acid (ASA) decreases this risk.3,4 The AHA guidelines state that medium dose ASA (30-50 mg/kg/d) can be used instead of the traditionally used high dose of 80-100 mg/kg/d as there is no evidence to suggest either dose is more effective.3 Medium to high-dose ASA usually is administered 4 times a day until the patient is afebrile then lowered to antiplatelet low-dose ASA of 3-5 mg/kg once daily.
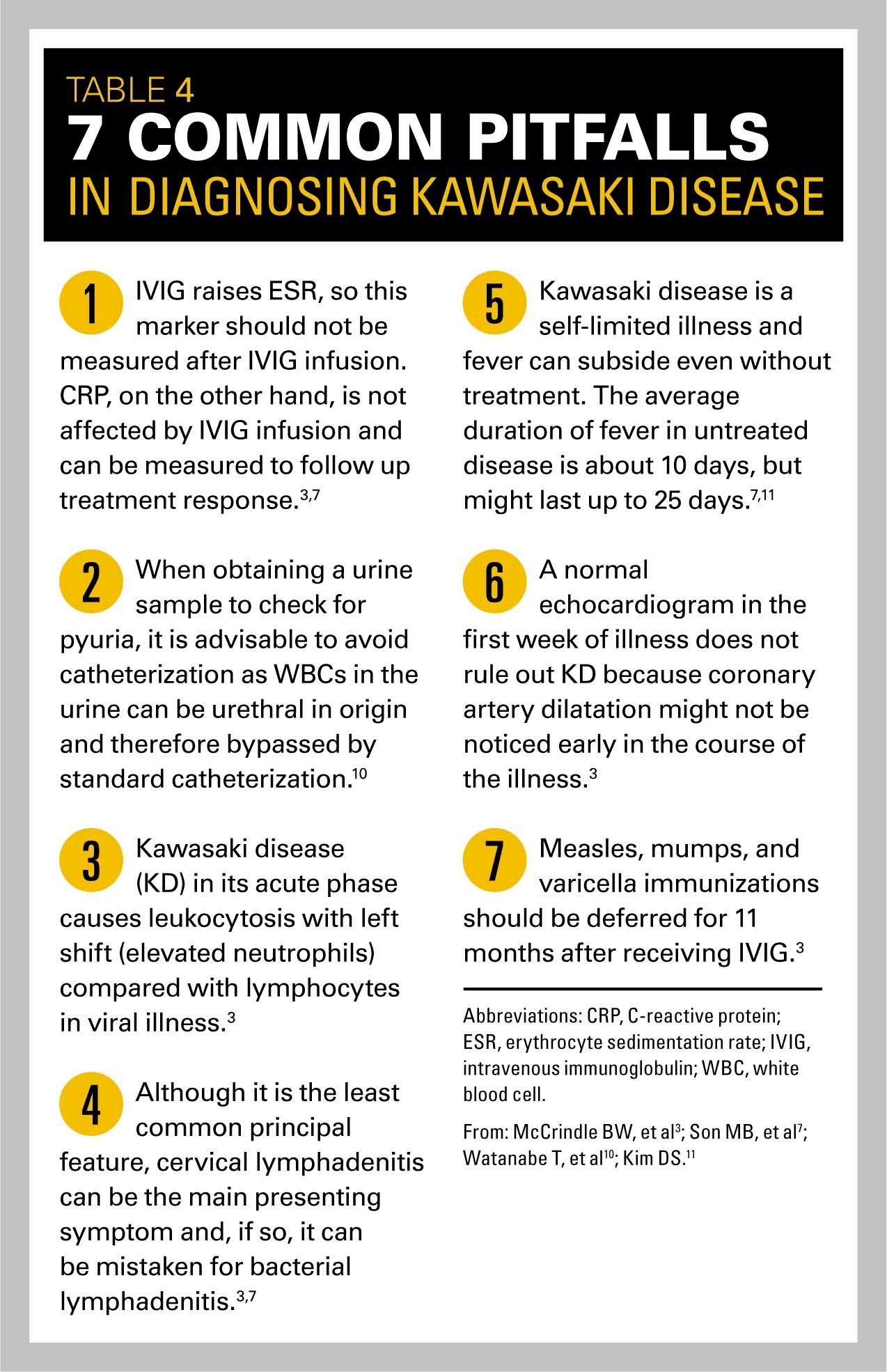
Other therapies include steroids, infliximab, and cyclosporine, but these usually are used in refractory cases and not routinely. Consultation with KD experts is always recommended in atypical or refractory cases.3,4,7 (See Table 4: Common pitfalls in diagnosing Kawasaki disease.)
Patient outcome
The patient was diagnosed with incomplete KD and received 1 dose of IVIG (2 g/kg) on day 8 of illness. His fever rapidly defervesced within 12 hours. He was started on high-dose aspirin (80 mg/kg/d). An echocardiogram showed normal cardiac structure and function with no coronary artery dilatations or aneurysms. The patient’s irritability resolved, and he was discharged home after 48 hours of being afebrile to follow up with Cardiology as an outpatient.
A follow-up echocardiogram 6 weeks after discharge revealed ectasia of the left main coronary artery, which confirmed the diagnosis of KD. No aneurysms were seen. The patient was maintained on daily aspirin and he continued to follow up with the Cardiology clinic. Of note, the patient in this case never developed oral changes, conjunctivitis, extremities changes (including skin peeling), or cervical lymphadenopathy.
Conclusion
Kawasaki disease in infants aged younger than 6 months requires a high index of suspicion for diagnosis as it can present only with prolonged fever and irritably without any other clinical features. This age group is at higher risk of delayed diagnosis and late treatment resulting in higher risk of CAAs. Intravenous immunoglobulin is an effective treatment and should be administered within 10 days of fever onset. A medium dose of ASA can be used instead of the high dose.
Next: Ears, nose, and throat, oh my!
Acknowledgement: The authors would like to thank Paige Triplett, DO, for her final review of this manuscript.
REFERENCES
1. Arora R, Mahajan P. Evaluation of child with fever without source: review of literature and update. Pediatr Clin North Am. 2013;60(5):1049-1062.
2. Antoon JW, Potisek NM, Lohr JA. Pediatric fever of unknown origin. Pediatr Rev. 2015;36(9):380-390.
3. McCrindle BW, Rowley AH, Newburger JW, et al; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Epidemiology and Prevention. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927-e999.
4. Dietz SM, van Stijn D, Burgner D, et al. Dissecting Kawasaki disease: a state-of-the-art review. Eur J Pediatr. 2017;176(8):995-1009.
5. Yeom JS, Woo HO, Park JS, Park ES, Seo JH, Youn HS. Kawasaki disease in infants. Korean J Pediatr. 2013;56(9):377-382.
6. Minich LL, Sleeper LA, Atz AM, et al; Pediatric Heart Network Investigators. Delayed diagnosis of Kawasaki disease: what are the risk factors? Pediatrics. 2007;120(6):e1434-e1440.
7. Son MB, Newburger JW. Kawasaki disease. Pediatr Rev. 2013;34(4):151-162.
8. Kawasaki T. Pediatric acute febrile mucocutaneous lymph node syndrome with characteristic desquamation of fingers and toes: my clinical observation of fifty cases. Pediatr Infect Dis J. 2002;21:1-38.
9. Yoon YM, Yun HW, Kim SH. Clinical characteristics of Kawasaki disease in infants younger than six months: a single-center study. Korean Circ J. 2016;46(4):550-555.
10. Watanabe T, Abe Y, Sato S, Uehara Y, Ikeno K, Abe T. Sterile pyuria in patients with Kawasaki disease originates from both the urethra and the kidney. Pediatr Nephrol. 2007;22(7):987-991.
11. Kim DS. Kawasaki disease. Yonsei Med J. 2006;47(6):759-772.
Boy presents with fatigue, minimal responsivity, and diffuse muscle weakness
August 7th 2024An 11-year-old boy with a history of asthma and allergic rhinitis presented to the emergency department (ED) with worsening fatigue, minimal responsivity to external stimuli, and diffuse muscle weakness for 2 months.
A 9-year-old boy presents with neck mass
July 3rd 2024A 9-year-old boy was seen for follow-up of a neck mass noted several years earlier. He first presented with this finding at 3 years of age, when during an otherwise unremarkable examination, he became upset, and a protuberant swelling was noted in the anterior aspect of the right side of his neck. What's the diagnosis?