Chronic cough in a 4-year-old boy
A previously healthy 4-year-old male, born late preterm by urgent cesarean delivery with an uncomplicated postnatal course, presents to the outpatient clinic for a chief complaint of worsening cough over the past 5 months. He denies current fever, rhinorrhea, shortness of breath, diarrhea, or vomiting. His cough has been worsening in severity and frequency, and mostly occurs during the daytime.
Figure 1
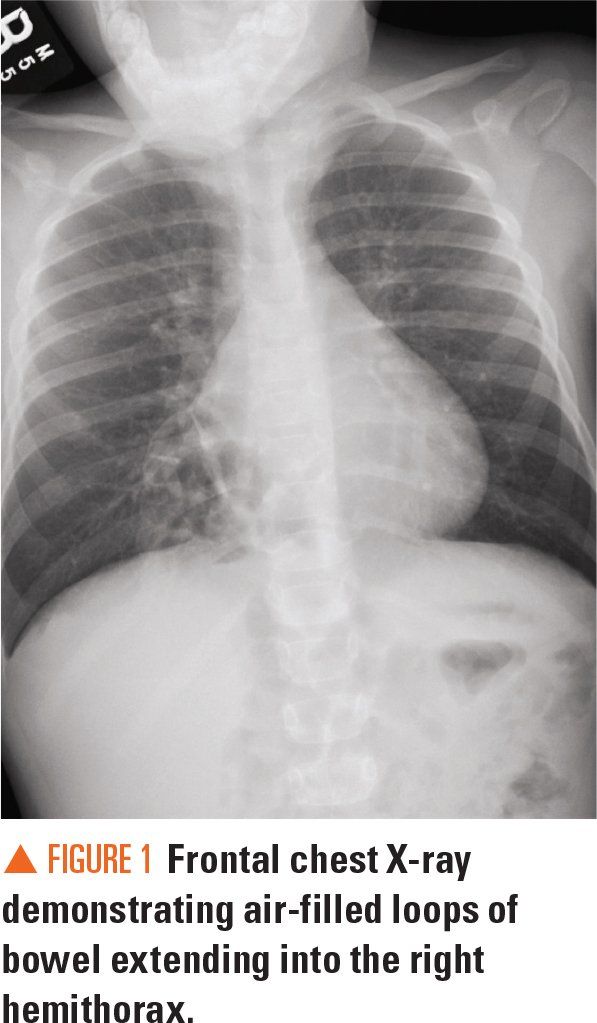
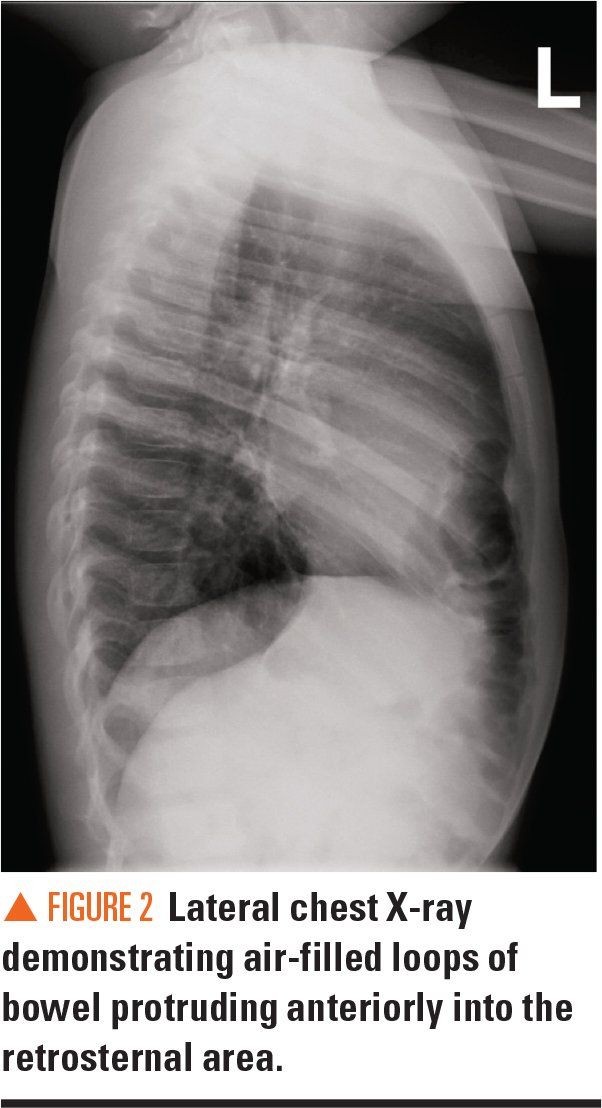
Figure 2
Differential diagnosis
The Case
A previously healthy 4-year-old male, born late preterm by urgent cesarean delivery with an uncomplicated postnatal course, presents to the outpatient clinic for a chief complaint of worsening cough over the past 5 months. He denies current fever, rhinorrhea, shortness of breath, diarrhea, or vomiting. His cough has been worsening in severity and frequency, and mostly occurs during the daytime. The cough does not worsen at night and does not interfere with the patient’s daily activities. The cough is nonproductive and is not exacerbated with activity or laying in the supine position. He does not have any sick contacts at home nor any history of recurrent viral upper respiratory infections.
History
The patient’s cough symptoms began 5 months ago when the patient was first seen in the emergency department (ED) for a viral upper respiratory infection (URI) and was prescribed Tylenol and ibuprofen. He was subsequently seen in the outpatient setting 2 more times for a persisting and worsening intermittent cough, where supportive care was recommended with a trial of Zyrtec, without symptomatic relief for the patient. Last week, he presented to immediate care for a 4-day history of cough, congestion, diarrhea and vomiting, and a 1-day history of fever. He was prescribed ibuprofen and supportive therapy for a presumed recurrent viral URI, and the majority of his symptoms resolved except for his cough, which continued to worsen and prompted evaluation at this visit.
Physical examination
On examination, the patient is a well-hydrated afebrile child in no acute distress. His growth parameters are normal for his age. His vital signs are all within normal limits, and he is saturating 98% oxygen on room air. He has moist mucous membranes without pharyngeal erythema or tonsillar exudates. He does not have cervical lymphadenopathy, pallor or cyanosis, and he is not tachypneic, wheezing, or in evident respiratory distress.
On auscultation, his lungs are clear bilaterally with good air movement, but bowel sounds are appreciated over his lower-right sternum. His abdomen is nontender, nondistended, with normoactive bowel sounds in all 4 quadrants.
Laboratory
During the patient’s visit to immediate care the previous week, urinalysis, rapid strep test, rapid influenza diagnostic testing, and a frontal chest X-ray to rule out pneumonia were obtained. Urinalysis was within normal limits, and both the influenza testing and rapid strep test results returned negative.
Imaging and consultation
The frontal chest X-ray demonstrated evidence of clustered gas collections at the gastroesophageal junction. Lateral and frontal chest X-rays were repeated at this visit, along with a respiratory polymerase chain reaction (PCR) panel. Respiratory PCR results were positive for parainfluenza. Both lateral and frontal chest X-rays demonstrated large air-filled loops of bowel extending anteriorly from the right diaphragm to medial right lower hemithorax (Figures 1 and 2). Pediatric surgery was consulted for evaluation of the abnormal imaging findings.
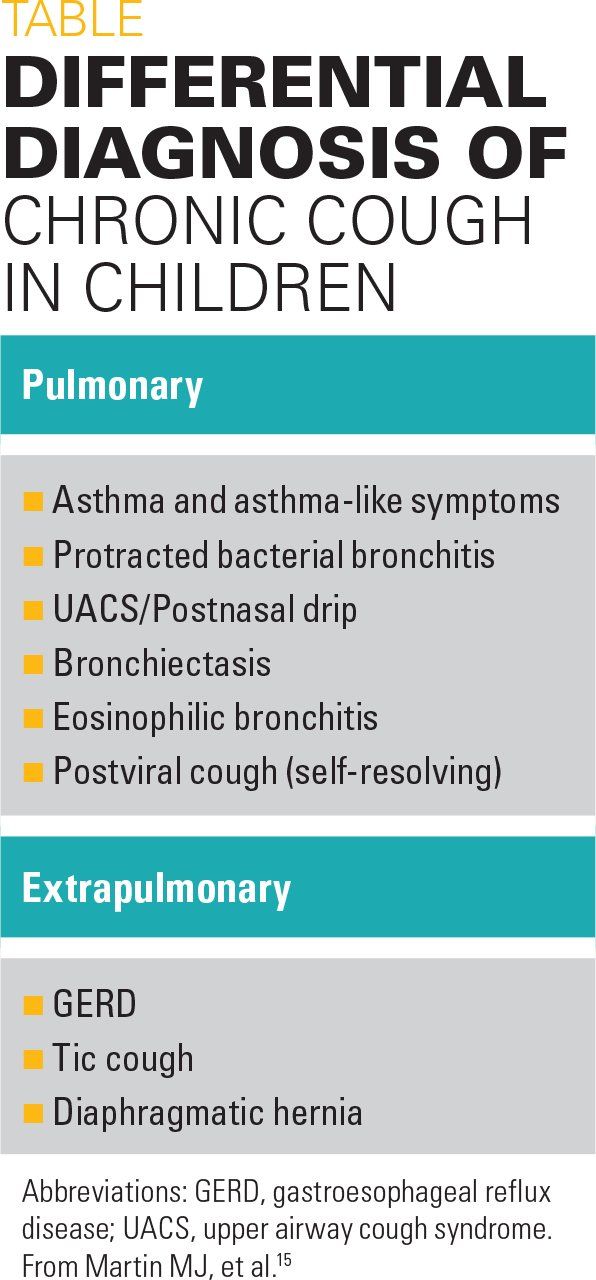
Differential diagnosis
Chronic cough in children is typically defined as a cough lasting longer than 4 weeks’ duration in a patient aged younger than 14 years.1 In 2 studies evaluating the etiologies behind chronic cough in children, the most common causes included upper airway cough syndrome (UACS), also known as postnasal drip; asthma and asthma-like symptoms; gastroesophageal reflux disease (GERD); and protracted bronchitis.2,3 Recommended initial evaluation in a child presenting with chronic cough is chest radiography and spirometry, although empiric therapy is usually not recommended in a child with a nonspecific chronic cough.1
For this patient, his first presentation was consistent with a viral URI, which appeared to be the precipitating event for his cough. While his cough persisted, this was thought to be a self-resolving postviral symptom or a recurrent viral URI. Of note, his viral respiratory PCR was positive for parainfluenza, which indicates that he did indeed have a viral URI at the time of presentation. A Morgagni hernia was detected incidentally on his chest X-ray for a workup of pneumonia when he presented to immediate care for a fever with chronic cough.
The patient’s worsening cough may have been exacerbated by his hernia contacting the pleura and pulmonary lining, which would have been already irritated from multiple viral URIs. Additionally, Morgagni hernias have been reported to present initially as repeated chest infections and gastrointestinal (GI) complaints,4 both of which were present in this patient. However, it is also a possibility that the cough worsened the extent of his hernia by increasing intraabdominal pressure and placing strain on the diaphragm.
Although imaging clearly demonstrated air-filled loops of bowel herniating through the patient’s diaphragm, imaging is not always definitive because the visualized bowel may vary in consistency. Oftentimes, further evaluation with a computed tomography (CT) scan is indicated to evaluate the extent of herniation and to rule out other causes such as a pericardial fat pad, lipoma, or mediastinal cyst.5
Although in many cases patients are asymptomatic, surgery is recommended on initial diagnosis of a Morgagni hernia to preserve normal lung function and prevent acute complications such as bowel incarceration.
Discussion
Congenital diaphragmatic hernia (CDH) occurs at a rate of fewer than 5 in 10,0000 births and is relatively rare compared with other potential etiologies of chronic cough. Most reported cases of CDH are Bochdalek hernias, which present via posterolateral defects in the diaphragm, whereas Morgagni hernias, which present anteromedially, are exceedingly rare, accounting for less than 5% of diagnosed CDHs.4 Interestingly, although cases of CDH classically present on the left hemisphere, Morgagni hernias frequently localize to the right hemisphere.
Whereas CDH typically presents postnatally as acute respiratory distress in the neonate, a small subgroup of patients with CDH present later in life and may be asymptomatic. Compared with Bochdalek hernias, Morgagni hernias are more likely to result in a delayed presentation and diagnosis.4 Also unlike Bochdalek hernias, Morgagni hernias are not associated with lung hypoplasia or pulmonary hypertension, and thus do not present with acute respiratory symptoms postnatally.
For patients with a delayed presentation of Morgagni hernia, common complaints included recurrent respiratory infections, nonspecific GI complaints, and failure to thrive. However, many Morgagni hernias are found incidentally on imaging.6 Acute symptoms such as neonatal respiratory distress and GI obstruction also have been reported.7,8 Morgagni hernias have been shown to be related to other congenital abnormalities, such as heart defects and chromosomal abnormalities.4
Morgagni hernias occur when the septum transversum fails to fuse with the costal arches during embryonic development, leading to a defect known as the foramen of Morgagni or the sternocostal triangle, which lies retrosternal, anteriorly and medially adjacent to the sternal and costal diaphragmatic attachments. Loops of large bowel, small intestine, or omentum subsequently can herniate through this open defect. The best initial imaging modality to diagnose a Morgagni hernia is chest radiograph in the postnatal period and beyond, which will demonstrate loops of bowel in the thoracic cavity, and ultrasound in the prenatal period, which will reveal a mass in the fetal thoracic cavity accompanied by a mediastinal shift.9
This case demonstrates the importance of a thorough physical exam, as not all diaphragmatic hernias present acutely or with obvious symptoms.
Management
Surgical repair is the first-line treatment following diagnosis of a Morgagni hernia. A transthoracic approach to the repair is preferred over a transabdominal approach because the transthoracic method offers adequate visualization and better control and avoids potential adhesions that may complicate a transabdominal approach.10 Reduction of hernia contents with primary closure is performed, oftentimes with a synthetic patch for larger defects and tension-free repair.11
A minimally invasive laparoscopic approach is also gaining favor, and is associated with a shorter operating time, shorter hospital length of stay, and a more pleasant cosmetic appearance.12 However, cases of hernia recurrence have been reported primarily in laparoscopic repairs without supportive prosthetic patches, and better visualization is obtained with an open approach.13 Open approaches are still more common than laparoscopic approaches.14
Lastly, as congenital heart defects and trisomy 21 are common comorbidities associated with Morgagni hernias, echocardiography and karyotype can be considered based on clinical suspicion.
Patient outcome
The patient was referred to pediatric surgery, where he underwent a laparoscopic repair of his Morgagni hernia with an uncomplicated operative and postoperative course. His chronic cough subsequently resolved after the hernia repair surgery.
References:
1. Chang AB, Oppenheimer JJ, Weinberger M, Weir K, Rubin BK, Irwin RS. Use of management pathways or algorithms in children with chronic cough: systematic reviews. Chest. 2016;149(1);106-119.
2. Karabel M, Kelekçi S, Karabel D, Gürkan MF. The evaluation of children with prolonged cough accompanied by American College of Chest Physicians guidelines. Clin Respir J. 2014;8(2),152-159.
3. Asilsoy S, Bayram E, Agin H, et al. Evaluation of chronic cough in children. Chest. 2008;134(6):1122-1128.
4. Al-Salem AH, Zamakhshary M, Al Mohaidly M, Al-Qahtani A, Abdulla MR, Naga M. Congenital Morgagni’s hernia: a national multicenter study. J Pediatr Surg. 2014;;49(4):503-507.
5. Minneci PC, Deans KJ, Kim P, Mathisen DJ. Foramen of Morgagni hernia: changes in diagnosis and treatment. Ann Thorac Surg. 2004;77(6):1956-1959.
6. Horton JD, Hofmann LJ, Hetz SP. Presentation and management of Morgagni hernias in adults: a review of 298 cases. Surg Endosc. 2008;22(6):1413-1420.
7. Griffiths EA, Ellis A, Mohamed A, Tam E, Ball CS. Surgical treatment of a Morgagni hernia causing intermittent gastric outlet obstruction. BMJ Case Rep. 2010;2010:bcr0120102608.
8. Wong NA, Dayan CM, Virjee J, Heaton KW. Acute respiratory distress secondary to Morgagni diaphragmatic herniation in an adult. Postgrad Med J. 1995;71(831):39-41.
9. Taylor GA, Atalabi OM, Estroff JA. Imaging of congenital diaphragmatic hernias. Pediatr Radiol. 2009;39(1):1-16.
10. Ambrogi V, Forcella D, Gatti A, Vanni G, Mineo TC. Transthoracic repair of Morgagni’s hernia: a 20-year experience from open to video-assisted approach. Surg Endosc. 2007;21(4):587-591.
11. Tsai J, Sulkowski J, Adzick NS, Hedrick HL, Flake AW. Patch repair for congenital diaphragmatic hernia: is it really a problem? J Pediatr Surg. 2012;47(4), 637-641.
12. Laituri CA, Garey CL, Ostlie DJ, Holcomb GW 3rd, St Peter SD. Morgagni hernia repair in children: comparison of laparoscopic and open results. J Laparoendosc Adv Surg Tech A. 2011;21(1):89-91.
13. Garriboli M, Bishay M, Kiely EM, et al. Recurrence rate of Morgagni diaphragmatic hernia following laparoscopic repair. Pediatr Surg Int. 2013;29(2):185-189.
14. Paul S, Nasar A, Port JL, et al. Comparative analysis of diaphragmatic hernia repair outcomes using the nationwide inpatient sample database. Arch Surg. 2012;147(7):607-12. Erratum in: Arch Surg. 2012;14i7(9):804.
15. Martin MJ, Harrison TW. Causes of chronic productive cough: an approach to management. Respir Med. 2015;109(9):1105-1113.
11-year-old boy with testicular pain and rash
January 19th 2024An 11-year-old boy presented to the emergency department complaining of left testicular pain for 2 days, described as intermittent and stabbing, which ranged between 5 and 8 of 10 in intensity. Read the full case to see if you can correctly diagnose the patient.
Newborn with midline neck lesion
December 21st 2023A 4-day-old boy with a midline neck lesion was born at term by normal vaginal delivery. After birth, mid line lesion had the configuration of a linear cleft with a cephalocaudal orientation, extending from the level below the hyoid bone to the suprasternal notch with a length of 2.5 cm and a width of 0.5 cm. What's the diagnosis?
A 13-year-old girl with well-demarcated rash on back and chest
October 19th 2023A healthy 13-year-old girl presented with a 1-month history of an asymptomatic, well-demarcated rash on her back and upper chest. The eruption consisted of discrete, dark brown papules that coalesced into large, flat-topped plaques with mild superficial scale and accentuation of skin markings. What's the diagnosis?
Suspicious facial swelling in a 22-month-old girl
October 11th 2023A 22-month-old female patient with sickle cell disease on folic acid and penicillin prophylaxis with a 3-day history of nasal congestion, rhinorrhea, fever and decreased oral intake presents to the emergency department (ED) for acute facial swelling noted when she woke up from a nap. What's the diagnosis?
Friction-induced blistering on a child’s feet
July 14th 2023You are called to the hospital nursery to evaluate a healthy full-term newborn boy who developed painful flaccid blisters and erosions on the tops of his feet and ankles shortly after birth. His mother had a history of similar recurrent skin lesions that healed with scarring. She also had oral and gastrointestinal tract involvement. What's the diagnosis?