Fever and neck swelling in a teenaged girl
A previously healthy 15-year-old female presents to the emergency department (ED) with complaints of right-sided neck swelling, pain, decreased range of motion, and fever for 3 days. She also reports a sore throat and mouth pain with decreased oral intake. She denies any rhinorrhea, shortness of breath, difficulty swallowing, vomiting, or dental pain. What's the diagnosis?
Table 1
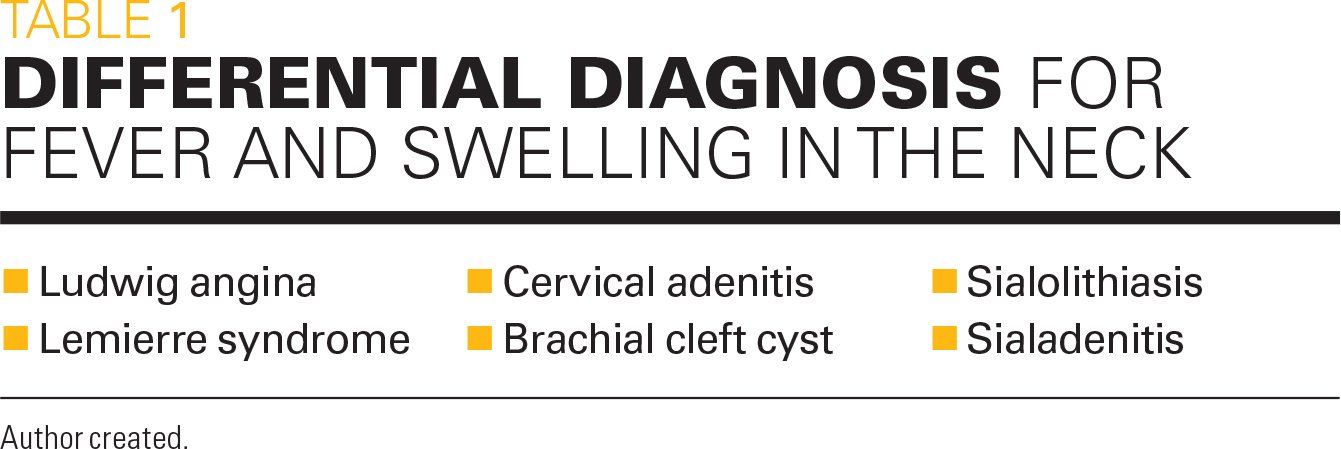
Table 2
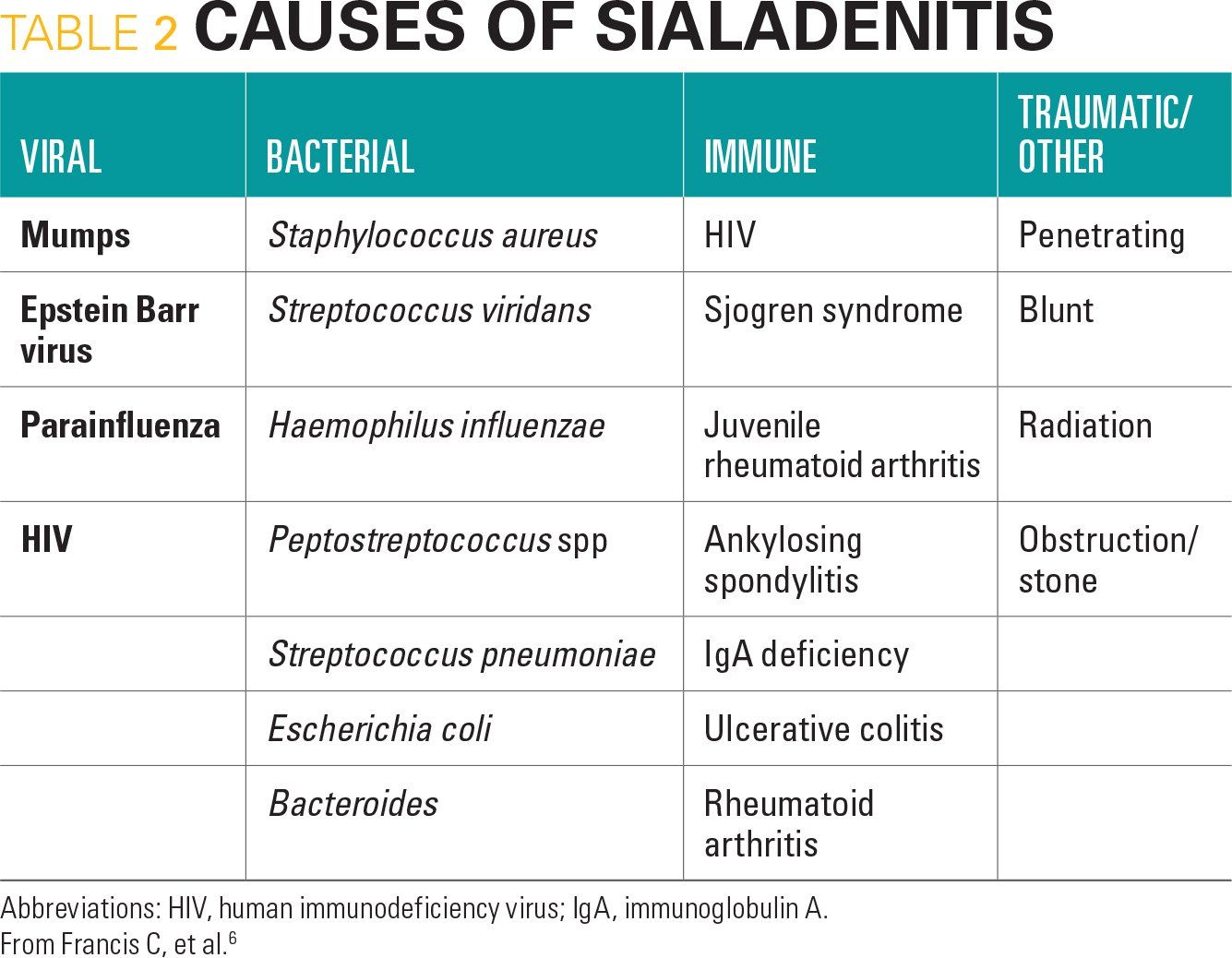
Figure 1
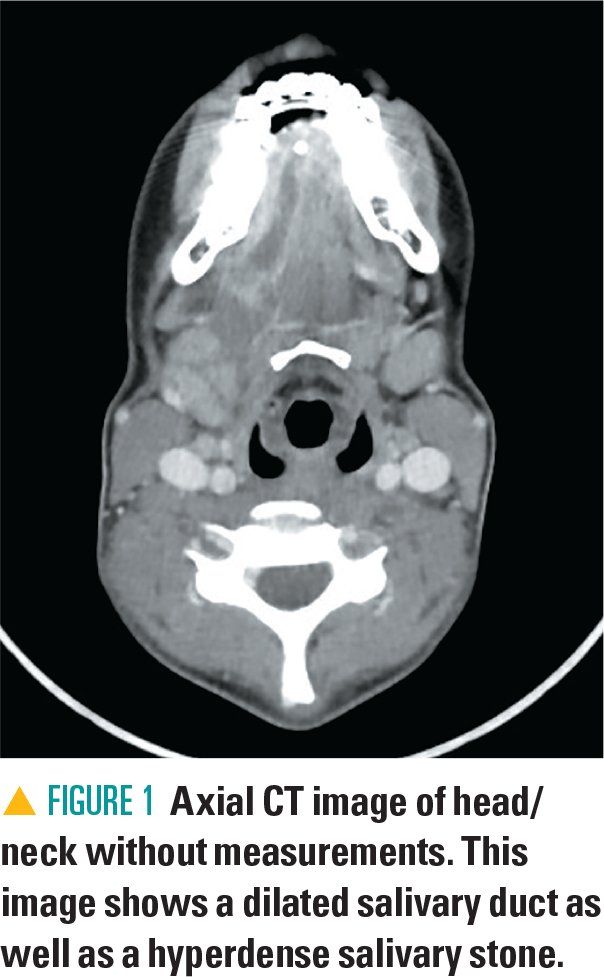
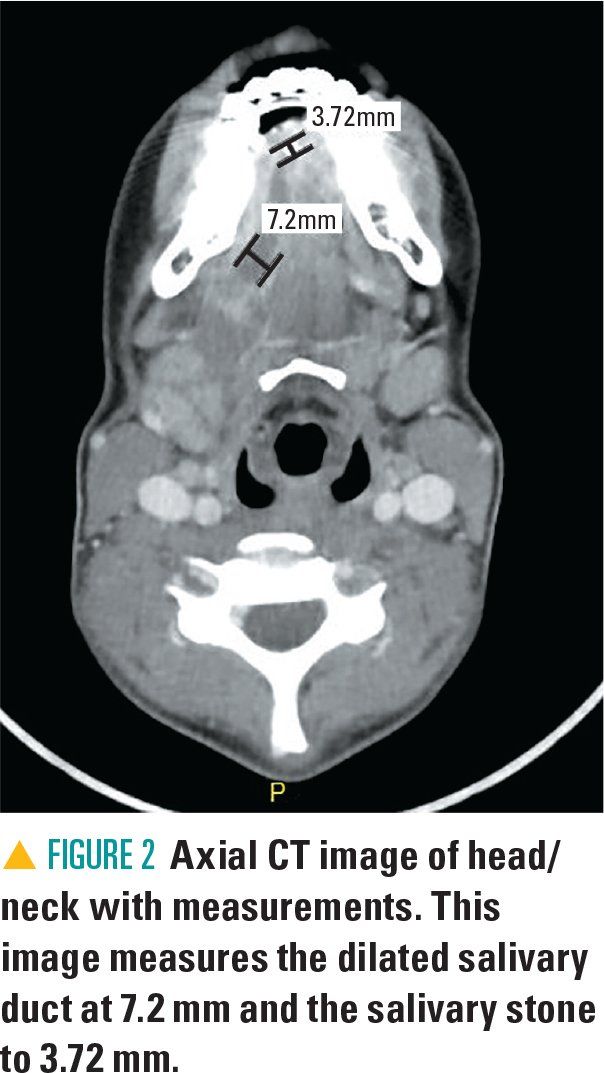
Figure 2
The case
A previously healthy 15-year-old female presents to the emergency department (ED) with complaints of right-sided neck swelling, pain, decreased range of motion, and fever for 3 days. She also reports a sore throat and mouth pain with decreased oral intake. She denies any rhinorrhea, shortness of breath, difficulty swallowing, vomiting, or dental pain.
The patient was previously evaluated by her primary care doctor earlier this same week with similar symptoms. She tested negative for mononucleosis and Streptococcus pharyngitis and was prescribed amoxicillin-clavulanate for suspected bacterial lymphadenitis. The parent and the girl report that the symptoms persisted and worsened despite the oral antibiotics. There is no other significant past medical history, family history, or surgical history.
Physical exam and lab tests
Upon arrival to the ED, the patient appeared to be in mild distress, secondary to pain. Her temperature was 98.6°F; pulse, 92 beats per minute; respiratory rate, 18 breaths per minute; blood pressure, 129/96 mm Hg; and oxygen saturation, 99% on room air. Her exam was significant for swelling at the floor of the mouth with no obvious dental caries or sources of infection. The right submandibular salivary gland was enlarged and tender to palpation. No overlying skin erythema was noted. The remaining physical exam was within normal limits.
Blood was obtained for analysis while the patient was in the ED and included a complete blood count, basic electrolytes, and inflammatory markers. Significant laboratory results included a total white blood cell count of 15,040 per mm3 with a differential count including 72% neutrophils. The C-reactive protein was elevated to 39.9 mg/L and erythrocyte sedimentation rate was 24 mm/h. The remaining laboratory values were normal.
Differential diagnosis
Differentials include Ludwig angina, Lemierre syndrome, cervical adenitis, brachial cleft cyst, sialadenitis, and sialolithiasis (Table 1). Ludwig angina is a form of cellulitis of the submental, sublingual, and submandibular spaces. Patients may present with swelling of the lower jaw and neck, mouth pain, and/or inability to open the mouth. This condition often spreads rapidly and can be life threatening due to the potential of upper airway obstruction.1 Ludwig angina is a rare diagnosis in the pediatric population, and because of the unfamiliarity of pediatric providers with the condition, children can potentially experience delay in diagnosis and treatment. This serious condition should be treated with intravenous antibiotic and possibly judicious surgical intervention.1
Lemierre syndrome is a rare type of oropharyngeal infection that is characterized by thrombosis of the internal jugular vein and multiple septic metastases/emboli.2 Patients with Lemierre syndrome often present with manifestations related to the primary infection such as fever, abdominal pain, nausea, vomiting, or cervical lymphadenopathy. The primary infection progresses to affect the parapharyngeal space invading the posterior compartment along the path of the carotid artery and ultimately leads to a thrombophlebitis of the internal jugular vein.2
Children with cervical adenitis may present with an acutely tender and inflamed cervical lymph node that will appear as neck swelling, similar to this case presentation. It is usually related to a recent upper respiratory infection and mainly affects the submandibular or anterior cervical lymph nodes.3 Pus is usually not visible in the roof of the mouth, unlike with sialadenitis.
Brachial cleft cysts may present as a painless, unilateral neck mass, unless they have become secondarily infected. Although present at birth, many cases of brachial cleft cysts do not become evident until later in childhood or adolescence.4
Finally, sialolithiasis are salivary stones that can occlude the salivary ducts and lead to inflammation and infection, or sialadenitis. These patients present with neck swelling, pain, fevers, and occasionally drainage from the salivary ducts. Sialolithiasis causing sialadenitis was diagnosed in this patient due to classic presentation and supporting lab work and imaging.
Diagnosis: sialadenitis and sialolithiasis
Sialadenitis is defined as inflammation of the salivary glands and can be caused by infection, obstruction, or less commonly autoimmune or allergic processes. Sialadenitis in the pediatric population accounts only for up to 10% of all salivary gland disease.5 A multitude of factors contribute to inflammation of the salivary glands including viral or bacterial infections, genetics, immunologic diseases, congenital abnormalities, dehydration, and allergies.6 Additional predisposing factors include sialolithiasis (or salivary stones), mucus plugs, stenosis, or foreign bodies.5 Sialolithiasis is a common etiology in the adult population. However, the prevalence of sialolithiasis in the pediatric population is thought to be as low as 3% of all cases.7
PATHOPHYSIOLOGY
Sialadenitis is a multifactorial process with multiple etiologies. Francis and Larsen composed a list of sialadenitis etiologies (Table 2) and included major causes such as viral, bacterial, immune, or traumatic.6 Prior to the measles/mumps/rubella (MMR) vaccine, viral sialadenitis was most commonly caused by mumps and affected the parotid gland. This has become less common with immunization efforts. Less common viral etiologies include Epstein-Barr virus (EBV), parainfluenza, and human immunodeficiency virus (HIV). Bacterial sialadenitis is most commonly caused by Staphylococcus aureus and Streptococcus species and presents with acute swelling, presence of pus, fever, and leukocytosis.8 Ductal stenosis can lead to obstructive sialadenitis and is more common in the parotid ductal system.9 Juvenile recurrent parotitis (JRP) is an important immunologic cause of sialadenitis and is thought to be the third-most common salivary disease in children, after mumps and viral infection.
While discussing sialolithiasis, it is important to understand the mechanism that leads to sialadenitis. Obstruction via a salivary stone causes inflammation, salivary stasis, postobstructive dilation, tissue damage, and remodeling that causes further inflammatory changes. Several theories have been proposed on how the salivary stone forms. One theory, proposed by Bodner and colleagues, states salivary mucin, bacteria, and desquamated epithelial cells form an initial organic nidus in which material deposits, forming a salivary stone.10,11 Another theory states the initiating factor is an infection, which changes salivary composition and leads to stone formation.12
The most common location for stone formation in the pediatric population is the submandibular gland. A study by Chung and colleagues of 29 pediatric patients demonstrated that the submandibular gland was affected in more than 90% of cases.12 This finding is similar to studies in adults. Another study by Lustmann and colleagues revealed the submandibular gland was affected in 94% of patients of all ages.7 Possible reasons why the submandibular gland is most often affected may be due to slower flow of secretions as well as higher calcium content.13 The parotid gland is the second-most common location and rarely the sublingual and minor salivary glands are involved.14 Sialolithiases in children are usually smaller, occur distally within the duct, and present with shorter symptoms duration.12,15
CLINICAL PRESENTATION
The clinical presentation of sialadenitis is consistent with the inflammatory state. The most common presenting symptom is swelling, followed by pain.7 Other symptoms include erythema, swelling associated with eating, and tenderness to palpation. Many times, purulence and/or mucus may be expressed by gentle manipulation of the gland and duct. In severe cases, systemic complications can extend into adjacent tissues or spread to distal sites.
DIAGNOSIS
Diagnosis of sialolithiasis/sialadenitis can be made by serology or gram stain when viral or bacterial etiologies are suspected. Imaging modalities may be necessary to rule out other life-threatening conditions such as Ludwig angina. These imaging modalities include plain radiographs, ultrasound, computed tomography (CT) with intravenous (IV) contrast, and sialography. In a retrospective case control study by Nahlieli and colleagues, 10 of the 15 cases (67%) of pediatric sialolithiasis were visible as radiopaque objects on radiographic film.15 However, up to 20% of submandibular salivary stones may be radiolucent on plain radiographs.11,16
Ultrasound can confirm the presence of an inflamed gland/duct, identify abscesses, and guide in aspiration, if clinically required.17 Computed tomography is the image modality of choice when abscess formation or systemic complications are suspected. However, information may be limited if the stones are smaller than 2 mm in size, and CT is often discouraged if the stone is palpable on exam.9 However, CT may be used for surgical planning for cases of salivary stones to detect the inflamed gland and identify the size, number of calculi, and location of the stones.17
Sialography is the gold study standard for evaluation of sialolithiasis. It is performed by injecting radiopaque dye into the intraductal system, followed by a plain radiograph. Sialograms are reported to be up to 100% effective in detecting ductal and intraglandular calculi. However, they are contraindicated in the acute phase as a sialogram is thought to aggravate the inflammatory state.8,18
MANAGEMENT
Treatment of sialadenitis is often conservative and targeted toward the suspected etiology. Sialolithiasis causing acute symptoms is initially managed conservatively with broad spectrum antibiotics, analgesics, hydration, warm massage, and sialagogues. Most common bacterial etiologies include gram-positive organisms whereas gram-negatives are less frequently seen. Therefore, penicillin derivatives and cephalosporins will provide appropriate coverage as first-line antibiotics.6 A list of likely organisms is shown in Table 2.
Spontaneous passage is more probable if the salivary stone is small and located in the distal section of the duct.16 In one study, the success rate with conservative management for a period of 3 months was only 10%.19
Surgical removal of salivary stones should be considered if conservative management fails. In a retrospective clinical review by Woo and associates, intraoral submandibular salivary stone removal led to complete recovery in 82.4% of pediatric patients.20 Salivary endoscopy has been validated in pediatrics as a safe and efficacious tool for the diagnosis and treatment of salivary gland disorders.9,15
Patient outcome
Because of the concern for Ludwig angina in this patient, which may also present with a painful neck swelling, a CT neck with contrast was ordered and was significant for obstructing sialolithiasis with a 4-mm stone and resulting sialadenitis involving the right submandibular gland and Wharton’s duct (Figures 1 and 2). Several small reactive lymph nodes were noted as well. Treatment with intravenous ampicillin-sulbactam was initiated and the patient was admitted to the pediatric ward for further therapy.
During her only day of hospitalization, therapy with intravenous antibiotics was continued as well as sialagogue agents such as sour candy that led to spontaneous expression of pus and drainage. Infectious Disease and Otolaryngology were consulted and recommended transitioning to oral therapy with oral clindamycin and referral for outpatient management. The patient was discharged with 600 mg of clindamycin every 8 hours and a follow-up appointment with Otolaryngology in 1 week.
At her follow-up appointment, the patient demonstrated persistent enlargement and pain. She was continued on clindamycin and scheduled for submandibular duct dilation and stone removal. About 2 weeks after initial admission, she underwent surgery with removal of a 0.2-cm x 0.2-cm x 0.2-cm stone. At her 1-week follow-up, there was no residual pain and the patient had made a full recovery.
Lessons for the clinician
Sialolithiasis and sialadenitis are rare conditions in the pediatric population. Although uncommon, these conditions represent unusual emergencies and should be diagnosed and treated in a timely fashion.
The treatment of sialolithiasis and sialadenitis is often conservative with antibiotics, analgesics, hydration, and sialagogue agents. However, failure of conservative therapy is an indication for surgical removal. Pediatric emergency physicians should suspect these diagnoses when the child presents with swelling, pain, erythema, and tenderness to palpation over the jaw or mouth. A Pediatric Otolaryngologist should be consulted early in the course of treatment.
ACKNOWLEDGMENT: The authors wish to thank Stacy McConkey, MD, FAAP, Medical Director of Pediatrics Program, Advent Health for Children, Orlando, Florida, for her contributions to this article.
References:
1. Chou YK, Lee CY, Chao HH. Upper airway obstruction emergency: Ludwig angina. Pediatr Emerg Care. 2007;23(12):892-896.
2. Garcia-Salido A, Unzueta-Roch JL, Garcia-Teresa MÃ, Sirvent-Cerdá S, Martinez de Azagra-Garde A, Casado-Flores J. Pediatric disseminated Lemierre syndrome in 2 infants: not too young for an ancient disease. Pediatr Emerg Care. 2017;33(7):490-493.
3. Margileth A. Cervical adenitis. Pediatr in Rev. 1985;7(1):13-24.
4. Chavan S, Deshmukh R, Karande P, Ingale Y. Branchial cleft cyst: a case report and review of literature. J Oral Maxillofac Pathol. 2014;18(1):150.
5. Jabbour N, Tibesar R, Lander T, Sidman J. Sialendoscopy in children. Int J Pediatr Otorhinolaryngol. 2010;74(4):347-350.
6. Francis CL, Larsen CG. Pediatric sialadenitis. Otolaryngol Clin North Am. 2014;47(5):763-778.
7. Lustmann J, Regev E, Melamed Y. Sialolithiasis: a survey on 245 patients and a review of the literature. Int J Oral Maxillofac Surg. 1990;19(3):135-138.
8. Brook I, Frazier EH, Thompson DH. Aerobic and anaerobic microbiology of acute suppurative parotitis. Laryngoscope. 1991;101(2):170-172.
9. Faure F, Querin S, Dulguerov P, Froehlich P, Disant F, Marchal F. Pediatric salivary gland obstructive swelling: sialendoscopic approach. Laryngoscope. 2007;117(8):1364-1367.
10. Bodner L, Azaz B. Submandibular sialolithiasis in children. J Oral Maxillofac Surg. 1982;40(9):551-554
11. McCullom C 3rd, Lee CY, Blaustein DI. Sialolithiasis in an 8-year-old child: case report. Pediatr Dent. 1991;13(4):231-233.
12. Chung MK, Jeong HS, Ko MH, et al. Pediatric sialolithiasis: what is different from adult sialolithiasis? Int J Pediatr Otorhinolaryngol. 2007;71(5):787-791.
13. Wallace E, Tauzin M, Hagan J, Schaitkin B, Walvekar RR. Management of giant sialoliths: review of the literature and preliminary experience with interventional sialendoscopy. Laryngoscope. 2010;120(10):1974-1978.
14. Bodner L, Fliss D. Parotid and submandibular calculi in children. Int J Pediatr Otorhinolaryngol. 1995;31(1):35-42.
15. Nahlieli O, Eliav E, Hasson O, Zagury A, Baruchin AM. Pediatric sialolithiasis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(6):709-712.
16. Williams MF. Sialolithiasis. Otolaryngol Clin North Am. 1999;32(5):819-834.
17. Orlandi MA, Pistorio V, Guerra PA. Ultrasound in sialadenitis. J Ultrasound. 2013;16(1):3-9.
18. Rice DH. Diseases of the salivary glands–non-neoplastic. In: Bailey BJ, Johnson JT, Kohut RI, et al, eds. Head and Neck Surgery-Otolaryngology. Vol 1. Philadelphia, PA: JB Lippincott; 1993:475-484.
19. Iro H, Zenk J, Koch M. Modern concepts for the diagnosis and therapy of sialolithiasis [article in German]. HNO. 2010;58(3):211-217.
20. Woo SH, Jang JY, Park GY, Jeong HS. Long-term outcomes of intraoral submandibular stone removal in children as compared with adults. Laryngoscope. 2009;119(1):116-120.

11-year-old boy with testicular pain and rash
January 19th 2024An 11-year-old boy presented to the emergency department complaining of left testicular pain for 2 days, described as intermittent and stabbing, which ranged between 5 and 8 of 10 in intensity. Read the full case to see if you can correctly diagnose the patient.
Newborn with midline neck lesion
December 21st 2023A 4-day-old boy with a midline neck lesion was born at term by normal vaginal delivery. After birth, mid line lesion had the configuration of a linear cleft with a cephalocaudal orientation, extending from the level below the hyoid bone to the suprasternal notch with a length of 2.5 cm and a width of 0.5 cm. What's the diagnosis?
A 13-year-old girl with well-demarcated rash on back and chest
October 19th 2023A healthy 13-year-old girl presented with a 1-month history of an asymptomatic, well-demarcated rash on her back and upper chest. The eruption consisted of discrete, dark brown papules that coalesced into large, flat-topped plaques with mild superficial scale and accentuation of skin markings. What's the diagnosis?
Suspicious facial swelling in a 22-month-old girl
October 11th 2023A 22-month-old female patient with sickle cell disease on folic acid and penicillin prophylaxis with a 3-day history of nasal congestion, rhinorrhea, fever and decreased oral intake presents to the emergency department (ED) for acute facial swelling noted when she woke up from a nap. What's the diagnosis?
Friction-induced blistering on a child’s feet
July 14th 2023You are called to the hospital nursery to evaluate a healthy full-term newborn boy who developed painful flaccid blisters and erosions on the tops of his feet and ankles shortly after birth. His mother had a history of similar recurrent skin lesions that healed with scarring. She also had oral and gastrointestinal tract involvement. What's the diagnosis?