How to integrate oral health into pediatric primary care: Part 1
Oral health screening performed at each well-child visit helps to identify oral disease or injury and promotes anticipatory guidance that can minimize caries risk and improve oral health outcomes.
Figures 1-6
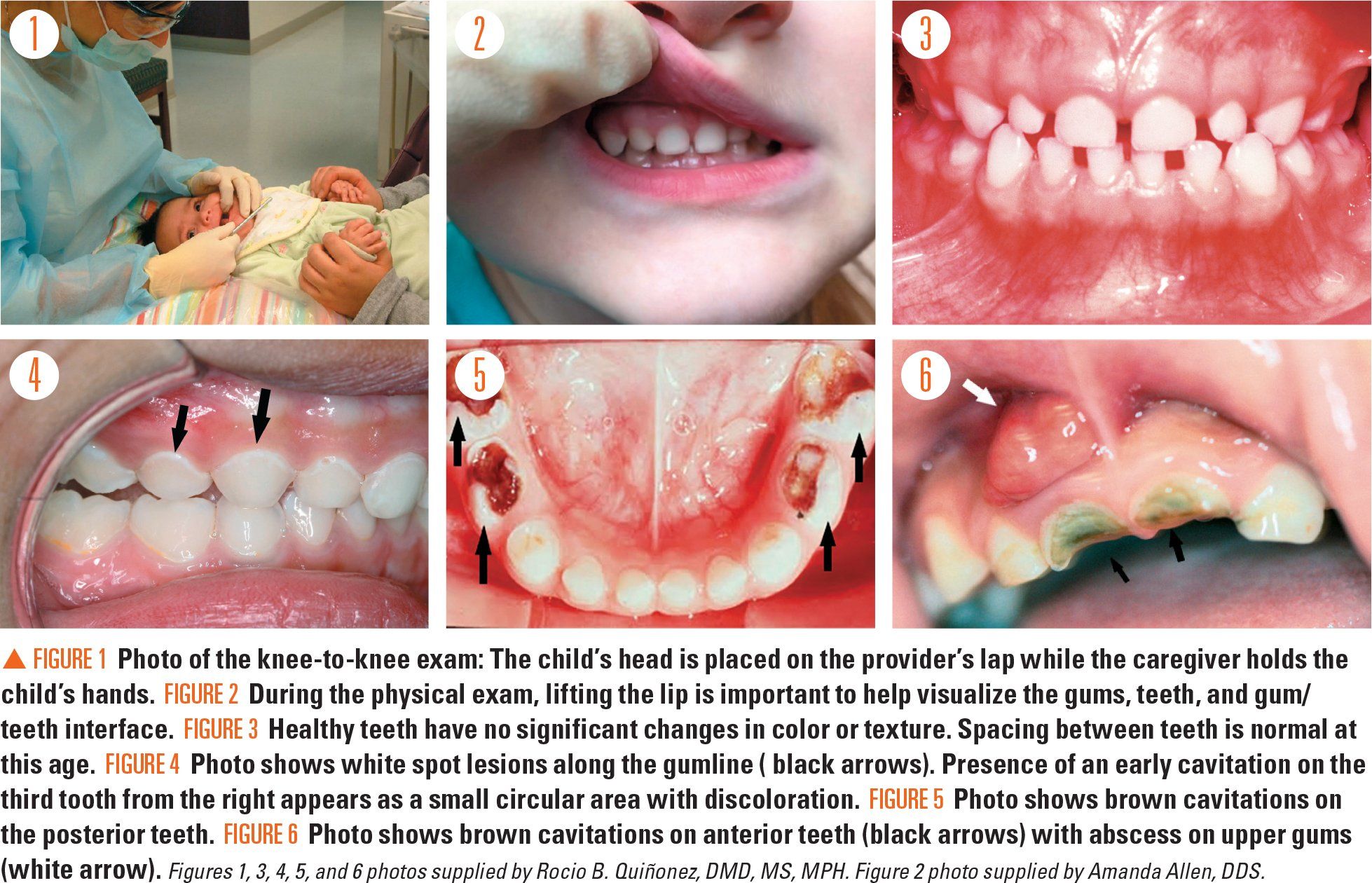
Table 1
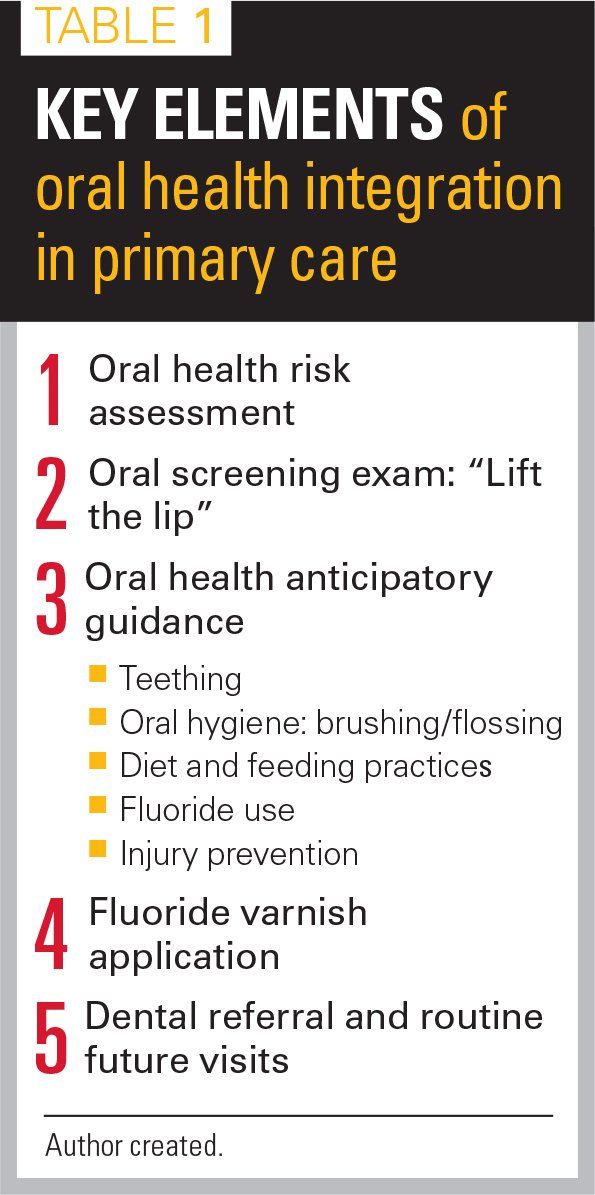
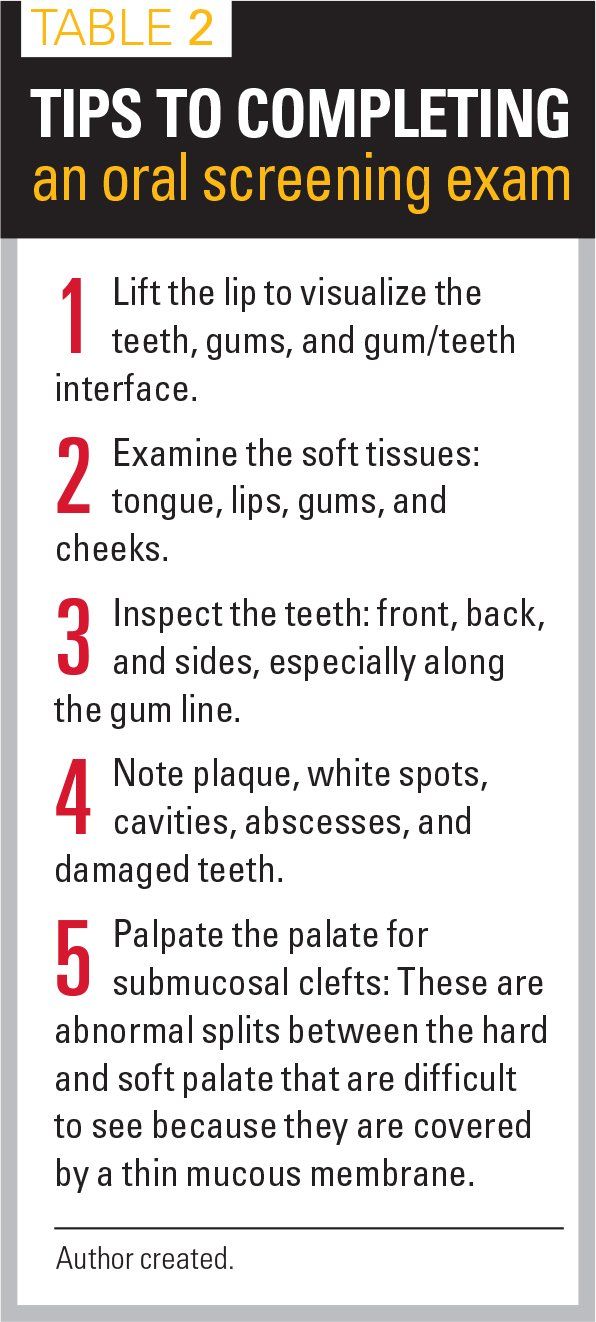
Table 2
Figures 7 and 8

Figure 9A and 9B
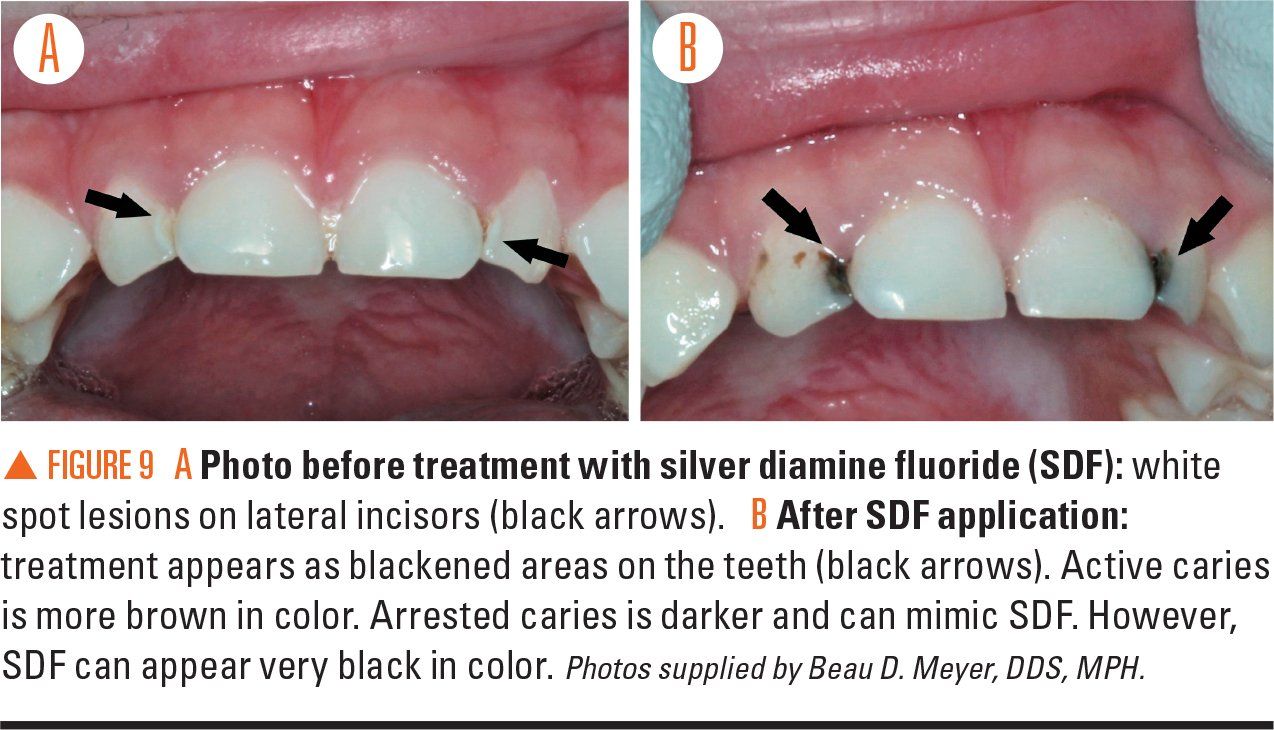
Table 3
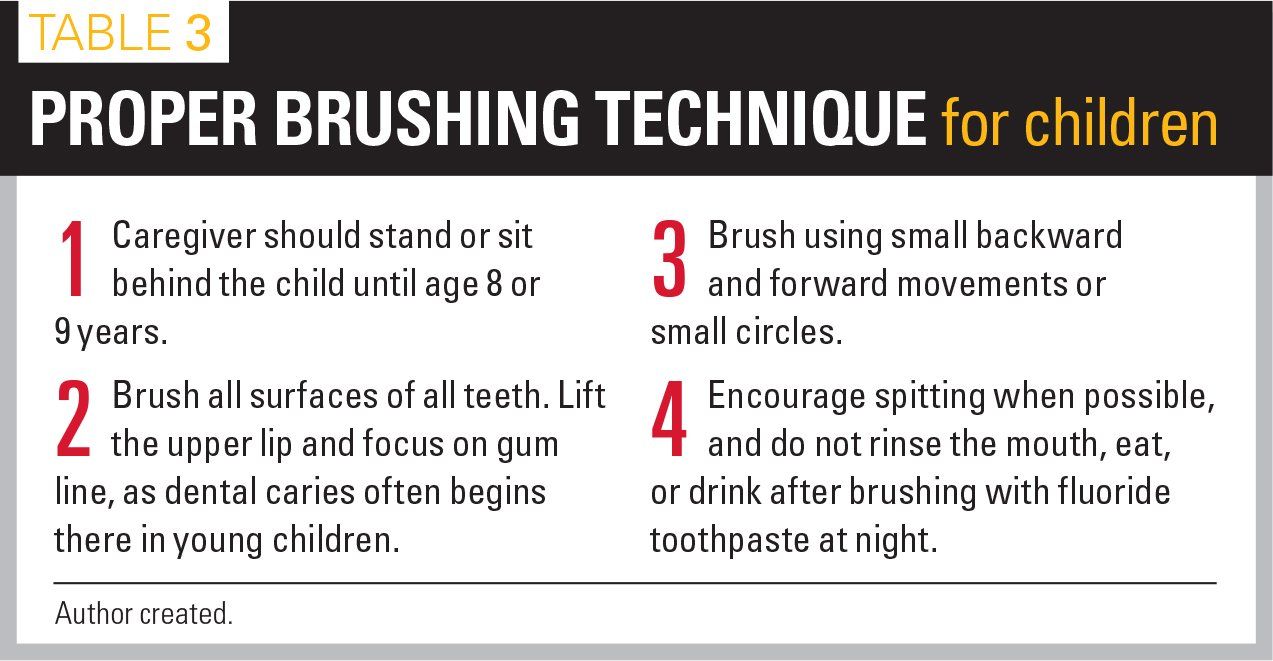
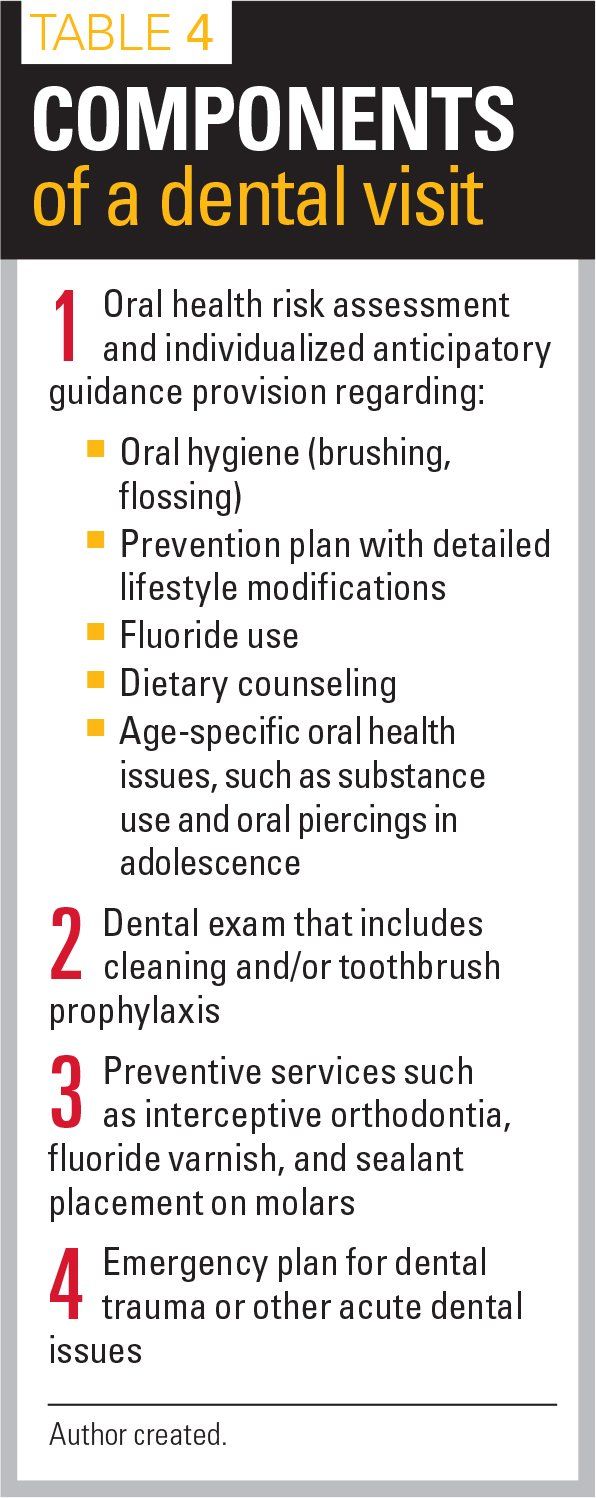
Table 4
Dental caries (cavities) continues to be the most common chronic disease in children1 with significant consequences including pain, infection, impaired growth, and frequent school absences. Caries is a multifactorial disease arising from the complex interplay of bacteria, dietary sugars, and teeth. The child, family, and larger community all influence caries risk and oral health outcomes.2 Pediatric primary care teams, a child’s first continuous exposure to healthcare, are well positioned to promote oral health during routine well child visits.
Oral health within the well-child visit
There are 5 key elements that should be integrated into the well-child visit (Table 1):
ORAL HEALTH RISK ASSESSMENT (OHRA)
To guide oral health discussion, an OHRA can be utilized starting at age 6 months. The American Academy of Pediatrics (AAP) OHRA is used in pediatric primary care to document a child’s risk factors, protective factors, and clinical findings, and to aid in provision of targeted anticipatory guidance.3 This OHRA identifies children who require urgent attention or more frequent dental visits.
ORAL SCREENING EXAM
The oral screening exam should be performed at each well-child visit and when indicated, such as following an injury or when child abuse is suspected. A systematic oral screening exam (Table 2) can identify and recognize oral disease and injury. In young children aged younger than 3 years, a knee-to-knee exam allows for a more controlled exam and improves exposure of the oral cavity (Figure 1).3
During the physical exam, lifting the lip can help to visualize the teeth, gums, and teeth/gum interface (Figure 2). In general, healthy teeth appear creamy white with no changes in color, roughness, or other irregularities (Figure 3). The first stage of dental caries is white spots and lines representing demineralized enamel (Figure 4). In children aged younger than 6 years, these lesions are called early childhood caries, an aggressive disease that requires urgent dental referral. All white spot lesions can progress to brown cavitations as enamel loss exposes the underlying yellow dentin (hard, dense tissue forming the bulk of a tooth; Figure 5). In severe dental caries, abscesses and/or fistulae may develop (Figure 6). Abscesses are painful, and the presenting signs in young nonverbal children may be decreased appetite, inability to chew, poor sleep, or irritability.
The clinical exam is also important to assess for injury of the soft or hard oral tissues. Injured teeth may be chipped, pushed forward/back or into the gum, or avulsed (knocked out). If the root of a primary tooth is injured, the tooth may turn brown or gray, cause pain, become infected, or require removal. Injured primary teeth can affect the development of underlying permanent teeth. In the case of a permanent tooth avulsion, the permanent tooth must be reimplanted immediately or as soon as possible for the greatest likelihood of tooth survival.4,5 Look for parallel placement, meaning that the crowns of the teeth should match to one another. Do not hold the tooth from the root surface as the periodontal ligament cells can be crushed and are needed for reattachment. If unable to insert in the socket, place tooth in milk. Water can lyse the cells and is not ideal. Primary teeth typically are not reimplanted.
Primary care clinicians also should be aware that 50% of injuries from child abuse occur in the mouth,6 and the oral cavity may be a focus of abuse because of its role in communication and nutrition. Craniofacial, head, face, and neck injuries are sustained in over one-half of child abuse cases, providing another impetus for a thorough oral examination.
ORAL HEALTH ANTICIPATORY GUIDANCE
Individualized oral health anticipatory guidance can minimize caries risk and improve health outcomes. Anticipatory guidance includes:
1. Teething: Discomfort associated with tooth emergence is a common concern. It is important to counsel that over-the-counter teething gels containing benzocaine are not recommended by the US Food and Drug Administration (FDA) because of potential for serious harm, including methemoglobinemia.7 Best practices for teething include massaging the gums with a wet washcloth or use of cool, solid (not fluid-filled) toys or teething rings that do not present a choking hazard. Oral pain medications, such as acetaminophen, should be used sparingly for severe pain.
2. Oral hygiene: Practices important in caries prevention include:
· Toothpaste use: Fluoride toothpaste should be used for all children, starting from tooth emergence.8 Do not recommend fluoride-free “training toothpaste.” From tooth emergence and until age 3 years, a grain of rice-sized (or “dab”) amount of fluoride toothpaste should be used to brush teeth morning and night (Figure 7). For children aged older than 3 years, or when a child can effectively spit, a pea-sized amount of fluoride toothpaste should be applied to the toothbrush (Figure 8). Children should be encouraged to spit after brushing, but recommended amounts of toothpaste are not expected to cause fluorosis if swallowed. Like all other medications, toothpaste should be kept out of reach of small children.
· Toothbrushing: Brush with proper technique (Table 3) for 2 minutes every morning and night using a soft bristled toothbrush. Children should be assisted with toothbrushing by an adult until aged 8 or 9 years. One effective AAP campaign encouraging brushing is “Brush, Book, Bed.”9 This campaign encourages families to have a nightly bedtime routine of brushing followed by reading a book and promoting a regular sleep time at night.
· Flossing: Flossing should begin at any age that teeth touch. The American Dental Association (ADA) recommends flossing once daily between teeth with an interdental cleaner.10 There is a clear disadvantage to leaving food stuck in teeth for long periods of time (including visual appearance and odor). Dexterity improves with maturity and flossing technique improves with practice.
3. Diet and feeding practices: Dietary choices influence overall health and dental caries risk. Oral health messaging will ideally begin prenatally, continue throughout pregnancy, and be emphasized with mothers on the postpartum unit because mothers want to know about all aspects of care of their newborn.11 Messaging during infancy should focus on encouraging breastfeeding, early cup introduction, discontinuing bottle use by aged 12 months (especially in bed), and recommending no fruit juice consumption during the first year of life.12 Messaging for older children includes choosing healthy beverages, especially plain water, and limiting carbonated and sugary beverages. Children should be encouraged to choose fresh fruits, vegetables, sugar-free whole-grain snacks, and to limit soda, candy, and sweets intake. Frequent intake of carbohydrates prevents neutralization of the acid produced by the oral bacteria by saliva3; therefore, eating should be limited to 3 meals per day and 1 snack between meals.
4. Fluoride use: Fluoride aids in caries prevention.13 Topical sources of fluoride including toothpaste, varnish, rinses, and fluoridated tap water provide the main effect of caries prevention by inhibiting tooth demineralization, enhancing tooth remineralization, and inhibiting local bacterial metabolism. The systemic mechanism of fluoride (through dietary supplements) has a lesser effect than the topical effect. Systemic fluoride is incorporated into the tooth matrix during tooth development to reduce enamel solubility and prevent enamel breakdown.14 The AAP and the US Preventive Services Task Force (USPSTF) recommend use of supplemental fluoride for children aged 6 months to 16 years if the drinking water is deficient in fluoride. Further discussion regarding fluoride modalities is forthcoming in part 2 of this article appearing in the February 2019 issue of Contemporary Pediatrics.
5. Injury prevention: Almost 30% of children sustain a tooth injury during childhood,15 with peak injuries occurring between ages 2 to 3 years in the primary dentition and 8 to 9 years in the permanent dentition. Injury prevention recommendations regarding young children include keeping one hand on infants in high places to prevent falls, avoidance of walker use, and car seats rear facing until the child is aged 2 years.16 Mouthguards are recommended for older children who engage in contact sports. Mouthguards decrease the risk of fractured teeth and lips, tongue, face, and jaw injuries. Three types of mouthguard protection are available17 including stock, boil-and-bite, and custom mouthguards, with the latter providing the best protection.
FLUORIDE VARNISH APPLICATION
Fluoride varnish is a highly concentrated form of topical fluoride that is applied to teeth during the clinical visit to inhibit or reverse white spot lesions on the teeth. The USPSTF recommends that primary care clinicians “apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption” through age 5 years.18 The varnish dose is 0.25 ml unidose 5% NaF (2.26% F) and frequency can range from every 3 to 6 months, based on the child’s caries risk considerations. A comprehensive discussion regarding fluoride varnish is included in the upcoming part 2 of this article in Contemporary Pediatrics, February 2019.
DENTAL REFERRALS/ROUTINE FUTURE DENTAL VISITS
Dental referrals are not just for urgent treatment. All children should be seen by a dentist (establish a dental home) by age 12 months19 or as soon as possible after age 1 year and then routinely throughout childhood and adolescence. Dental referral is required for definitive treatment once a specific need has been identified.
Over the past decade, medical and dental community collaboration has increased referral of children for dental care. Early dental visits may decrease cost, lessen need for subsequent dental procedures,20 and enhance future preventive dental visits.21 Families should be informed of what to expect at dental visits (Table 4).
Once a specific need has been identified, treatment occurs in the dental setting. Early cavities may be stabilized using fluoride-releasing restorative materials. Severe dental caries may require fillings and/or root canals, crowns, or tooth extraction with placeholders for permanent teeth eruption. The latter procedures often require use of sedation or general anesthesia with increased cost and risk of adverse events.
Silver diamine fluoride (SDF) is a newer modality to treat primary tooth cavities. It consists of a liquid containing silver particles that is applied to a cavity and acts as a physical barrier, provides antibacterial properties, and contains fluoride to strengthen enamel. The disadvantage is permanent black discoloration of the treated tooth surface (Figures 9A and 9B); therefore, SDF is used most often to stabilize cavities in primary teeth and in children with increased risk for harm from an invasive dental procedure.22
Oral health integration
Primary care office flow may require adjustment to integrate oral health into clinical practice and encourage dental referrals.23 A template placed in the electronic medical record (EMR) for oral health evaluation can prompt clinicians to provide appropriate guidance at the clinic24 while encouraging fluoride varnish application and dental referrals.
Medical-dental integration can be further fostered by primary care practices reaching out to community dental providers to collaborate on oral healthcare practices. This bidirectional relationship will lead to consistent messaging from all healthcare professionals. It may be helpful to distribute a list of local dental providers who accept specific insurances and/or create a dental referral form for use in the practice.25 In addition, identification of an oral health champion within a clinical care setting or the local community can further promote ongoing education and sustained advocacy to promote oral health integration into office practice.
In summary
Oral health is an important aspect of overall health. Prevention by primary care clinicians should focus on risk assessment, oral examination, provision of age-appropriate anticipatory guidance (oral hygiene, home fluoride use, fluoride varnish application, dietary counseling, injury prevention) and early dental referral while encouraging routine dental care.
For information, see modules 2 and 6 of the Smiles for Life curriculum,26www.smilesforlifeoralhealth.org.
References:
1. Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;(248):1-92.
2. Fisher-Owens SA, Gansky SA, Platt LJ, et al. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120(3):e510-e520.
3. American Academy of Pediatrics. Oral health practice tools. Available at: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Oral-Health/Pages/Oral-Health-Practice-Tools.aspx. Accessed January 2, 2019.
4. Keels MA; Section on Oral Health, American Academy of Pediatrics. Management of dental trauma in a primary care setting. Pediatrics. 2014;133(2):e466-e476.
5. Kinirons MJ, Gregg TA, Welbury RR, Cole BO. Variations in the presenting and treatment features in reimplanted permanent incisors in children and their effect on the prevalence of root resorption. Br Dent J. 2000;189(5):263-266.
6. Fisher-Owens SA, Lukefahr JL, Tate AR. Oral and dental aspects of child abuse and neglect. Pediatr Dent. 2017;39(4):278-283.
7. US Food and Drug Administration. Risk of serious and potentially fatal blood disorder prompts FDA action on oral over-the-counter benzocaine products used for teething and mouth pain and prescription local anesthetics. Available at: www.fda.gov/Drugs/DrugSafety/ucm608265.htm. Published May 23, 2018. Accessed January 2, 2019.
8. American Dental Association Council on Scientific Affairs. Fluoride toothpaste use for young children. J Am Dent Assoc. 2014;145(2):190-191. Erratum in: J Am Dent Assoc. 2014;145(3):236.
9. Barone LF. Brush, Book, Bed-3 simple steps to good oral health and improved literacy. Pediatrics. 2018;141(1 Meeting Abstract):597.
10. American Dental Association. Federal government, ADA emphasize importance of flossing and interdental cleaners. Available at: https://www.ada.org/en/press-room/news-releases/2016-archive/august/statement-from-the-american-dental-association-about-interdental-cleaners. Published August 4, 2016. Accessed January 2, 2019.
11. Hallas D. Fernandez JB, Lim LJ, et al. (2015). OHEP: an oral health education program for mothers of newborns. J Pediatr Health Care, 2015;29(2):181-190.
12. Heyman MB, Abrams SA; Section on Gastroenterology, Hepatology, and Nutrition; Committee on Nutrition. Fruit juice in infants, children, and adolescents: current recommendations. Pediatrics. 2017;139(6):e20170967.
13. Clark MB, Slayton RL; Section on Oral Health. Fluoride use in caries prevention in the primary care setting. Pediatrics. 2014;134(3):626-633.
14. Weyant RJ, Tracy SL, Anselmo TT, et al; American Dental Association Council on Scientific Affairs Expert Panel on Topical Fluoride Caries Preventive Agents. Topical fluoride for caries prevention: executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc. 2013;144(11):1279-1291.
15. Andersson L. Epidemiology of traumatic dental injuries. Pediatr Dent. 2013;35(2):102-105.
16. Casamassimo P, Holt K, eds. Bright Futures: Oral Health-Pocket Guide. 3rd ed. Washington, DC: National Maternal and Child Oral Health Resource Center; 2016.
17. Gould TE, Piland SG, Caswell SV, et al. National Athletic Trainers’ Association position statement: preventing and managing sport-related dental and oral injuries. J Athl Train. 2016;51(10):821-839.
18. Moyer VA; US Preventive Services Task Force. Prevention of dental caries in children from birth through age 5 years: US Preventive Services Task Force recommendation statement. Pediatrics. 2014;133(6):1102-1111. Available at: www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/dental-caries-inchildren-from-birth-through-age-5-years-screening. Published May 5, 2014. Accessed January 2, 2019.
19. American Academy of Pediatric Dentistry Council on Clinical Affairs. Policy on the dental home. Pediatr Dent. 2018;40(6):29-30..
20. Nowak AJ, Casamassimo PS, Scott J, Moulton R. Do early dental visits reduce treatment and treatment costs for children? Pediatr Dent. 2014;36(7):489-493.
21. Savage MF, Lee JY, Kotch JB, Vann WF Jr. Early preventive dental visits: effects on subsequent utilization and costs. Pediatrics. 2004;114(4):e418-e423.
22. Fung MHT, Duangthip D, Wong MCM, Lo ECM, Chu CH. Randomized clinical trial of 12% and 38% silver diamine fluoride treatment. J Dent Res. 2018;97(2):171-178.
23. Hummel J, Phillips KE, Holt B, Hayes C. Oral Health: An Essential Component of Primary Care. Seattle, WA: Qualis Health; June 2015.
24. American Academy of Pediatrics Section on Oral Health. Key elements to incorporate oral health in the pediatric electronic health record. Available at: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Oral-Health/Documents/EMRTemplate.pdf. Accessed January 2. 2019.
25. American Academy of Pediatrics Section on Oral Health. Dental referral resource template. Available at: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Oral-Health/_layouts/15/WopiFrame.aspx?sourcedoc=/en-us/advocacyand-policy/aap-health-initiatives/Oral-Health/Documents/Dental-Referral-Resource-Template.doc&action=default. January 2, 2019.
26. Clark MB, Douglass AB, Maier R, et al. Smiles for Life: A National Oral Health Curriculum. 3rd ed. Society of Teachers of Family Medicine. 2010. Available at: www.smilesforlifeoralhealth.com. Accessed January 2, 2019.