The Dx of ADHD
Attention-deficit/hyperactivity disorder (ADHD) was first recognized over 100 years ago, but the diagnostic criteria has changed over the years. Here's a look at the latest guidance for diagnosing ADHD.
History and introduction
The condition we now refer to as attention-deficit/hyperactivity disorder (ADHD) was first recognized in England in 1902 by eminent physician Dr George Still (eg, Still’s Disease = Juvenile Rheumatoid Arthritis). Dr Still identified and reported in the journal Lancet several boys who seemed normal physically and intellectually but who struggled with symptoms of “restlessness, inattention, and hyper-arousal.” The cause was then unknown.
Following the pandemic of influenza in 1918, similar findings in children and adolescents were labeled “post-encephalitic syndrome” or “minimal brain damage,” later changed to “minimal brain dysfunction” when no obvious brain deficits were noted. Hyperactivity also led to the term “the hyperactive child.” Essentially, all the cases were male.
In the 1980s, emphasis was placed on the most universal trait, inattentiveness, and the term attention deficit disorder (ADD) was adopted. This gave rise to the diagnosis in females, who, though often “fidgety” are usually not grossly “hyperactive.” The Diagnostic and Statistic Manual of Mental Disorders, Fourth Edition (DSM-IV) distinguished 3 subtypes: inattentive only, hyperactive/impulsive only, and combined type, (inattentive, hyperactive, and impulsive), and changed the terminology to ADHD.
The Diagnostic and Statistic Manual of Mental Disorders, Fifth Edition (DSM-5), published in 2013, made these changes in diagnostic criteria: (paraphrased). 1) ADHD was defined as a “neurodevelopmental disorder” rather than a “neurobehavioral disorder,” putting emphasis on the developmental rather than the behavioral, opening the door for educational interventions, as well as other advantages. 2) For adolescents aged 17 years and older, and adults, only 5 out of the 9 criteria for inattention, or hyperactivity/impulsivity are required for diagnosis, versus 6 in DSM-IV. 3) Several of the inattentive/hyperactive/impulsivity symptoms must present before age 12. (DSM-IV required symptoms prior to age 6: Females a year after 6, more likely to be the inattentive type, often did not meet diagnostic criteria. 4) DSM-5 specified that ADHD may coexist with a diagnosis of autistic spectrum disorder (ASD) since some children have overlapping symptoms, allowing more clarity of diagnosis, and therapeutic options.
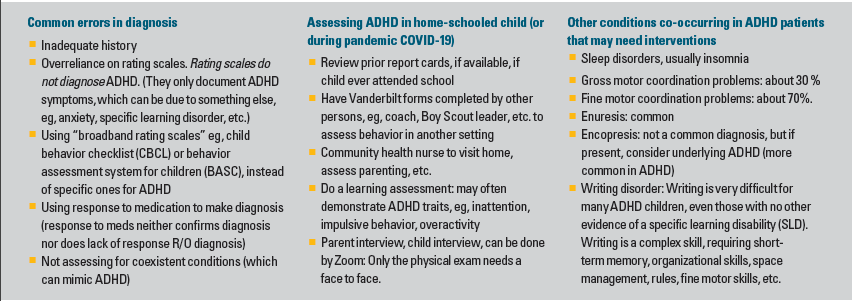
Common errors in diagnosis
The American Academy of Pediatrics, who had initially published Guidelines for Diagnosis and Treatment of ADHD in 2011, published a guideline update in November 2019.1 Though the earlier guidelines were not significantly altered, the following rules were re-emphasized: (paraphrased)
1. Any child aged 4-18 years, who manifests academic or behavioral issues, symptoms of inattention, and/or hyperactivity/impulsivity, should be assessed for ADHD.
2. To make a diagnosis, the primary care clinician (PCC) should verify that DSM-5 symptom criteria have been met, to a degree causing impairment, including documentation of symptoms in at least 2 environments (eg, school, home), as reported by caregivers, teachers or other school personnel, and/or mental health persons involved in the child’s care.
3. The evaluation for ADHD should include a screening process to rule out other comorbid conditions (see table) which can “mimic” the symptoms of ADHD, or be a coexistent condition. (Note: studies have shown that as many as 75% of children/adolescents diagnosed with ADHD fulfill criteria for another DSM-5 condition, such as specific learning disorder (SLD), anxiety, and/or depression, oppositional defiant disorder, etc. The term “ADHD Complex” is now being used to describe those children/adolescents.)
4. Since ADHD is a chronic condition, the PCC should manage the child in the same manner used to manage any child with special care needs, using the principles of the chronic care model.
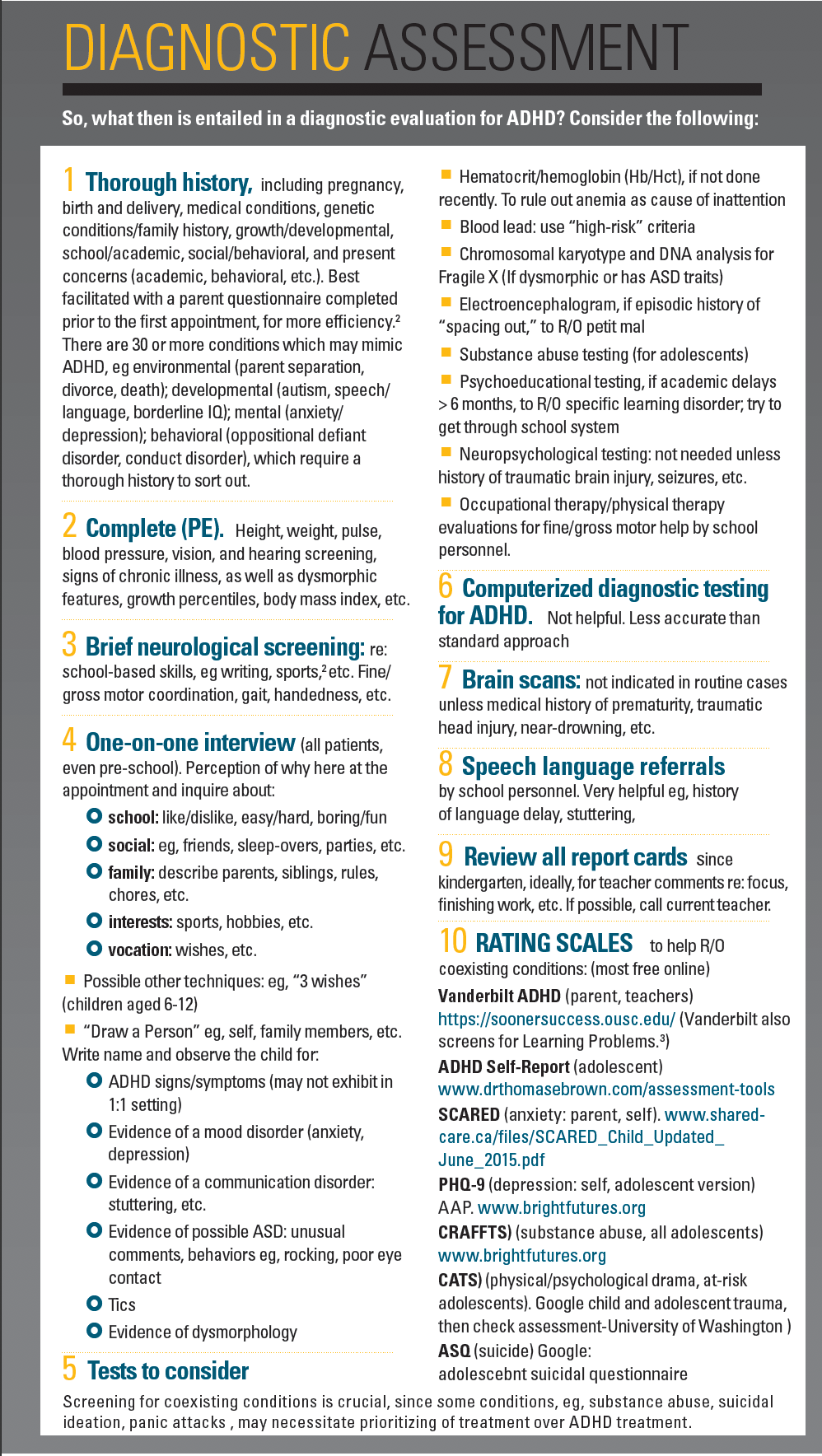
Diagnostic assessment for ADHD
Miscellaneous “pearls” re: diagnosing
Pre-school child: can be challenging to diagnose accurately, eg, mistaken for delayed maturational skills versus inadequate parenting. Always withhold diagnosis until parents have attended a thorough parenting class or 1:1 parenting help and are practicing good parenting skills. If significant improvement, perhaps is not ADHD. Lack of adequate response to behavioral interventions can then lead to consideration of medication trial and presumptive diagnosis of ADHD.
Phone call to teacher. Invaluable. An experienced teacher can be extremely helpful to help decide whether child’s inattention is due to learning difficulty or more boredom/disinterest? (than ADHD).
Thorough medical history, as noted earlier: There are 30 or more conditions that can cause symptoms which mimic ADHD.2
- Medical: eg, obstructive sleep apnea, traumatic brain injury, lead, medications, hypoxemia, near-drowning, prematurity etc.
- Developmental: eg, ASD, SLD, speech/language disorders, lower IQ
- Environmental: eg, abuse, neglect, death in family, divorce/separation
- Mental/behavioral: eg, anxiety, depression, trauma
About 2/3 of children/adolescents diagnosed with ADHD are combined typed (mostly males) and 1/3 are females, mostly inattentive type. Males are often diagnosed early, in kindergarten or first grade due to overactivity and impulsive behavior. Girls are frequently not diagnosed until later eg, start of middle school, when they fail to turn in assignments in a timely manner.
In July 2016 the US Department of Education classified ADHD as a “specific disability” under the Civil Rights Law, which helps obtain special services for children and adolescents with ADHD.
The proper testings/screenings, of course, are only half the battle. However, once a conclusive diagnosis of ADHD has been made, there are a number of medications and tools to help your child navigate the healthiest and happiest childhood and adolescence possible (see “The Rx of ADHD”).
References
1) Wolraich ML, Hagan, JF, Allan C, et al. Clinical practice guidelines for the diagnosis, evaluation, and treatment of attention deficit/hyperactivity disorder in children and adolescents. Pediatrics. October 2019;144(4). doi:10.1542/peds.2019-2528
2) Gephart H. ADHD Complex: Practicing Mental Health in Primary Care. Elsevier Publishing; 2019. https://doi.org/10.1016/c2018-0-00447-8
3) Langberg JM et al. Clinical utility of the Vanderbilt ADHD Rating Scale for ruling out comorbid learning disorders. Pediatrics. October 2010;126(5).
doi:10.1542/peds.2010-1267
Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.