Treating an 18-month-old who tested positive for cannabis exposure
As more and more states legalize recreational marijuana, caregivers need to be vigilant about keeping products out of reach of children.
Clinical vignette
An 18-month-old boy presented to the pediatric emergency department (PED) with a chief concern of unresponsiveness. Emergency Medical Services called ahead to inform the PED staff that they were bringing in the child who had been found unresponsive at home. Report given in transit stated that the patient had normal vital signs and was breathing on his own but was difficult to wake and that there were several sick individuals in the home.
Upon arrival, the child was placed in the resuscitation room, and a broad workup was initiated, including a complete metabolic panel, venous blood gas, blood and cerebrospinal fluid cultures, respiratory viral testing, and head computed tomography. Additionally, serum acetaminophen, salicylate, and ethanol levels were drawn and a standard 7-drug urine drug of abuse screen test administered. The physical exam was notable for a sedated child with upper extremity rigidity and shaking. Pupils varied between mydriasis and miosis. The patient received naloxone 2 mg intravenous (IV) with no effect, a meningitis dose of ceftriaxone, and a total of 60 mL/kg IV fluids. The parents arrived approximately 20 minutes after the patient and were interviewed. Initial blood glucose of the child was 120 mg/dL, and the family denied he could have gotten into any substances at home.
The child had no significant past medical history. The family had been sick and been taking over-the-counter cough and cold syrups and ibuprofen. The grandmother also lived with the family and noted that she had antidiabetic medications. The urine collected approximately 4 hours after presentation was positive for delta-9-tetrahydrocannabinol (THC). The results were discussed with the caregivers. At that time, the grandmother reported cannabis products in the home. The patient returned to baseline about 6 hours after presenting to the PED and was discharged home.
Epidemiology of use and legalization
After alcohol, cannabis is the most widely used mind-altering substance in the United States. Recent survey data suggests a rise in use within the home that coincides with the legalization of marijuana for medical or recreational use.1 As of December 2022, 47 states and the District of Columbia regulate cannabis. Idaho, Nebraska, and Kansas do not.2
Changes in pediatric exposure
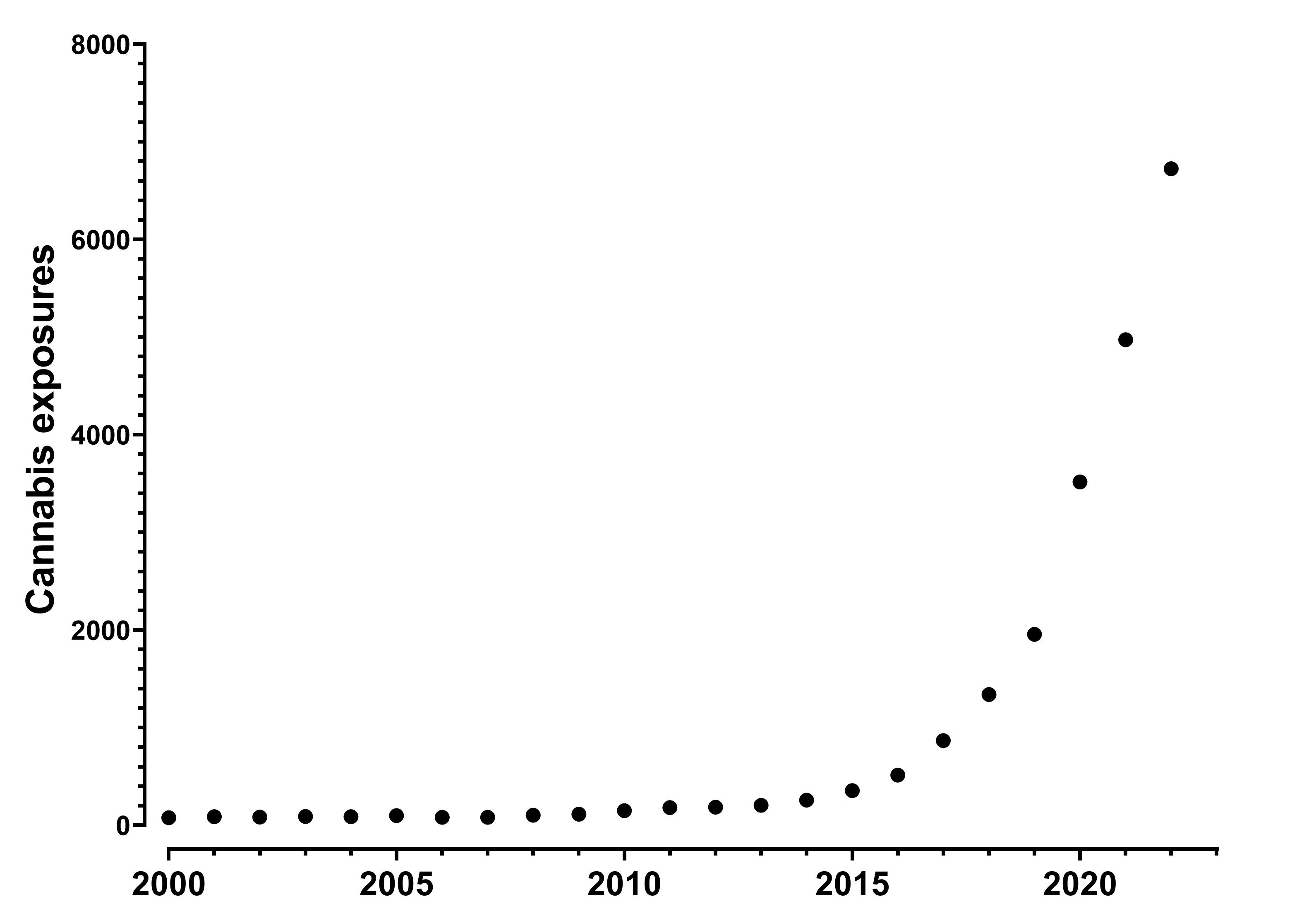
Recent studies using US poison center data showed significant increases in non-misuse or abuse exposures in young children.3 From 2000 through 2013, all cannabis exposure in children aged 0 to 12 years old increased a small amount per year. From 2014 through 2019, exposures increased from about 450 to 2400 per year, and in 2020 the figure rose to approximately 4500 (Figure).3 A focused analysis of the years 2017 through 2020 found a sharp increase in monthly exposures beginning in April of 2020, consistent with lockdowns.4
This increase is not unique to the US. Researchers from Ontario, Canada, reported increased emergency department visits in children aged 0 to 9 years after the legalization of cannabis flower and an even greater one after the legalization and sale of edibles.5
Edibles
Hundreds of edible cannabis products are available commercially. They include soda, chocolate bars, gummies, candies, chips, brownies, cookies, crispy rice and marshmallow bars, among others. One survey reported that 8% (n=13) of edibles came in packaging that was nearly identical to that of non–THC containing products.6 Several products used the exact brand and product names and imitated multiple components of non–cannabis containing products packaging (labels, font, colors, logos). All but one listed the total THC content per package, with a mean of 459 mg, which is well above the threshold to cause THC intoxication irrespective of user weight.6 Edible cannabis products are available at dispensaries. Although federal law prohibits interstate commerce in cannabis, some dispensaries offer same-day delivery.
Figure: Cannabis exposures reported to United States Poison centers in children ages 0-12 years old. Includes all forms of cannabis.
Clinical course
Children who have ingested cannabis edibles typically present with central nervous system (CNS) depression ranging from lethargy to coma.7 Common CNS effects include ataxia, confusion, agitation, and tremors. One study analyzed approximately 7,000 cases of cannabis exposure reported to United State Poison Centers from 1/1/2000 through 12/31/2020.3 Patients were age 0 to 12 years and seen in a healthcare facility. Tachycardia and vomiting were common and reported in 10% of these exposures. Seizures occurred in 1%, hypotension in 1.5%, and bradycardia in 1.1%. Respiratory depression was reported in up to 2.2%, but 0.7% of patients were intubated. Metabolic derangements are uncommon, although some patients may develop hypoglycemia if they are too fatigued to maintain oral intake. Decreased oral intake should prompt blood glucose testing. Otherwise, no routine blood testing is required for management, but urine testing can confirm the diagnosis.
Symptom duration may be prolonged in many cases. In a systematic review, the duration of symptoms ranged from 6 to 48 hours.7 There is no antidote for THC intoxication. Many patients do not need specific treatments and are monitored in the emergency department or general medical floor. Only a small portion of patients admitted to the intensive care unit (ICU) receive interventions specific to the ICU. Children may be too lethargic to eat. They may also be agitated and need frequent reassurance or sedation.
Management
A key to the diagnosis of any poisoning is to inquire about the toxin availability in the home. As described in the clinical vignette, these children may arrive without a history of ingestion. They may have CNS depression, variations in muscle tone, tachycardia, and tremors. The onset is rapid (<2 hours), and many patients have a clearly defined last known well time. In published case reports and series, many patients have undergone several diagnostic tests, including computed tomography and lumbar puncture.7 One study reported an increase in tests and overall costs of testing when no history of exposure was reported.8 The urine drug screen is a reasonable test in a child with altered mental status with or without a confirmed history of ingestion.
Early identification of possible exposure to cannabis products may help guide diagnostic screening and treatments in the emergency department. The combination of a positive THC result on urine toxicology screening ruling out other potential causes, may reduce admissions to the ICU after cannabis ingestion. Published data suggest only a small proportion of the patients admitted to the ICU receive interventions limited to the ICU. Many of these patients can be observed on the floor or in the emergency department and be discharged once they return to baseline and a safe discharge can be arranged. Counsel caregivers on poisoning prevention. This includes purchasing and storing product in a locked container, ensuring products are put away immediately after use, and disposing of them in non-visible garbage cans.
Conclusion
The legalization of cannabis for recreational and medical use, especially in the form of edibles, has been associated with increased pediatric exposures. Consider the diagnosis of a cannabis ingestion in children with abrupt onset of altered mental status and send urine drug screen as part of the broad workup for children presenting this way. Care is primarily supportive and assistance for prognosis, monitoring, and treatment is available 24/7/365 from your local poison center at 800-222-1222.
References
1. Goodwin RD, Kim JH, Cheslack‐Postava K, et al. Trends in cannabis use among adults with children in the home in the United States, 2004–2017: impact of state‐level legalization for recreational and medical use. Addiction. 2021;116(10):2770-2778. doi:10.1111/add.15472
2. National Conference of State Legislatures. State Medical Cannabis Laws. September 12, 2022. Accessed December 8, 2022. https://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx
3. Leonard JB, Laudone T, Hines EQ, Klein-Schwartz W. Critical care interventions in children aged 6 months to 12 years admitted to the pediatric intensive care unit after unintentional cannabis exposures. Clin Toxicol (Phila). 2022;60(8):960-965. doi:10.1080/15563650.2022.2059497
4. Laudone TW, Leonard JB, Hines EQ, Seung H, Klein-Schwartz W. Changes in unintentional cannabis exposures in children 6 months to 5 years reported to United States poison centers during the first nine months of the Coronavirus-19 pandemic. Clin Toxicol (Phila). 2022;60(9):1029-1031. doi:10.1080/15563650.2022.2064867
5. Myran DT, Cantor N, Finkelstein Y, et al. Unintentional pediatric cannabis exposures after legalization of recreational cannabis in Canada. JAMA Netw Open. 2022;5(1):e2142521. doi:10.1001/jamanetworkopen.2021.42521
6. Ompad DC, Snyder KM, Sandh S, et al. Copycat and lookalike edible cannabis product packaging in the United States. Drug Alcohol Depend. 2022;235:109409. doi:10.1016/j.drugalcdep.2022.109409
7. Richards JR, Smith NE, Moulin AK. Unintentional cannabis ingestion in children: a systematic review. J Pediatr. 2017;190:142-152. doi:10.1016/j.jpeds.2017.07.005
8. Bashqoy F, Heizer JW, Reiter PD, Wang GS, Borgelt LM. Increased testing and health care costs for pediatric cannabis exposures. Pediatr Emerg Care. 2021;37(12):e850-e854. doi:10.1097/PEC.0000000000001811

Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.
Full case: Infant presents with an asymptomatic pearl-like nodule on the heel
Infant is closely monitored at subsequent well visits and rechecked after 3 months, showed full resolution of the skin lesion over the heel area.
Diagnose this infant with an asymptomatic pearl-like nodule on the heel
Can you diagnose this patient? Take our poll and find out! Then check back for the full case, differential diagnosis, and correct diagnosis.