Young woman with tick bites presents with erythematous papules, headaches, and fatigue
A young woman with no significant past medical history returns from hiking with several white-spotted ticks and experiences erythematous papules, rashes, headaches, and fatigue. What’s the diagnosis?
The case
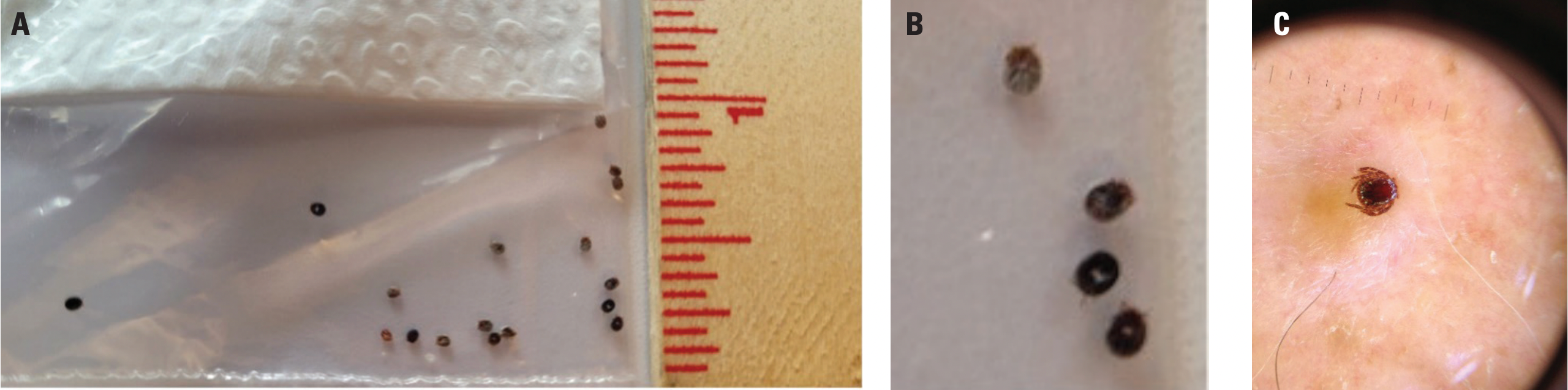
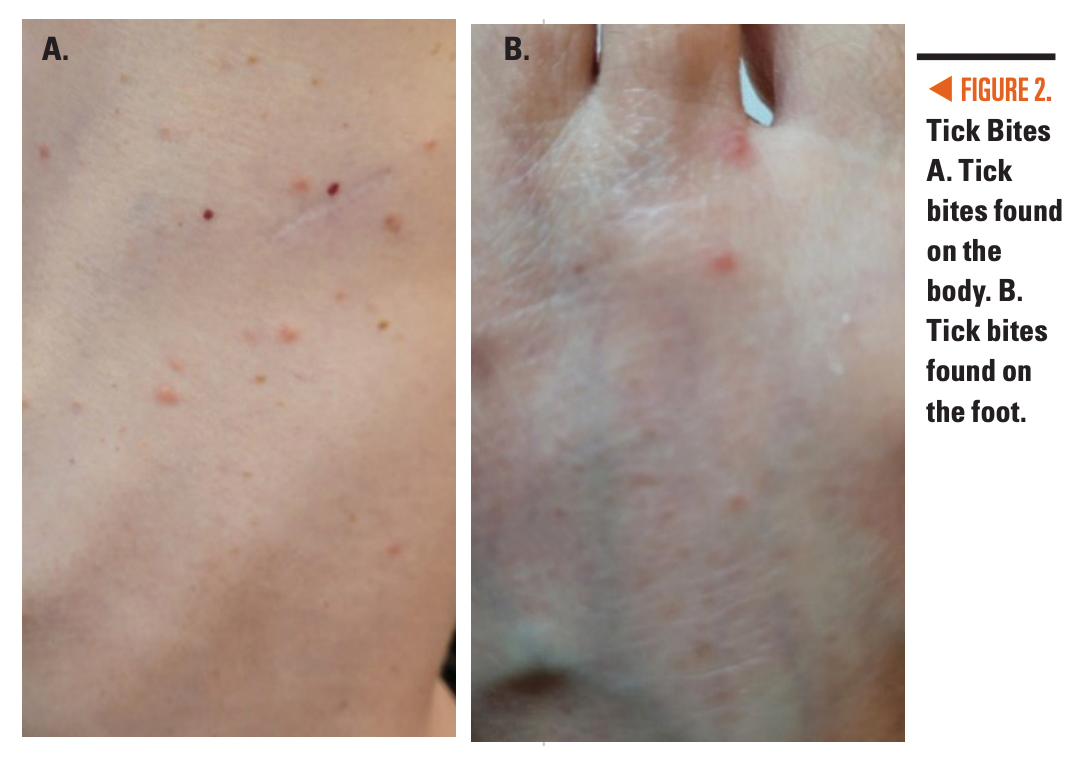
A young woman with no significant past medical history was walking her dog in the woods in a state park in the metropolitan area of Washington, DC. When she woke up the next morning, she found multiple ticks on her bedsheet and pulled over 30 ticks off her back, many of which had white spots on their backs (Figure 1). She had red papules 2 to 3 mm in diameter all over her body, particularly on her back, hands, and feet (Figure 2). A rash around her navel appeared 3 days later. For 2 to 3 weeks, she experienced headaches and fatigue as well as soreness under her armpit and a red sandpaper rash but no fever.
FIGURE 1. A.) Multiple ticks. B. Female ticks. C. Male tick. Click image to enlarge.
Differential diagnosis
This patient with no prior medical history presented with widespread red erythematous papules,many in a linear pattern, as well as erythema and scaling, fatigue, headaches, and arthralgias, but no fever. She found several ticks with white spots on them.
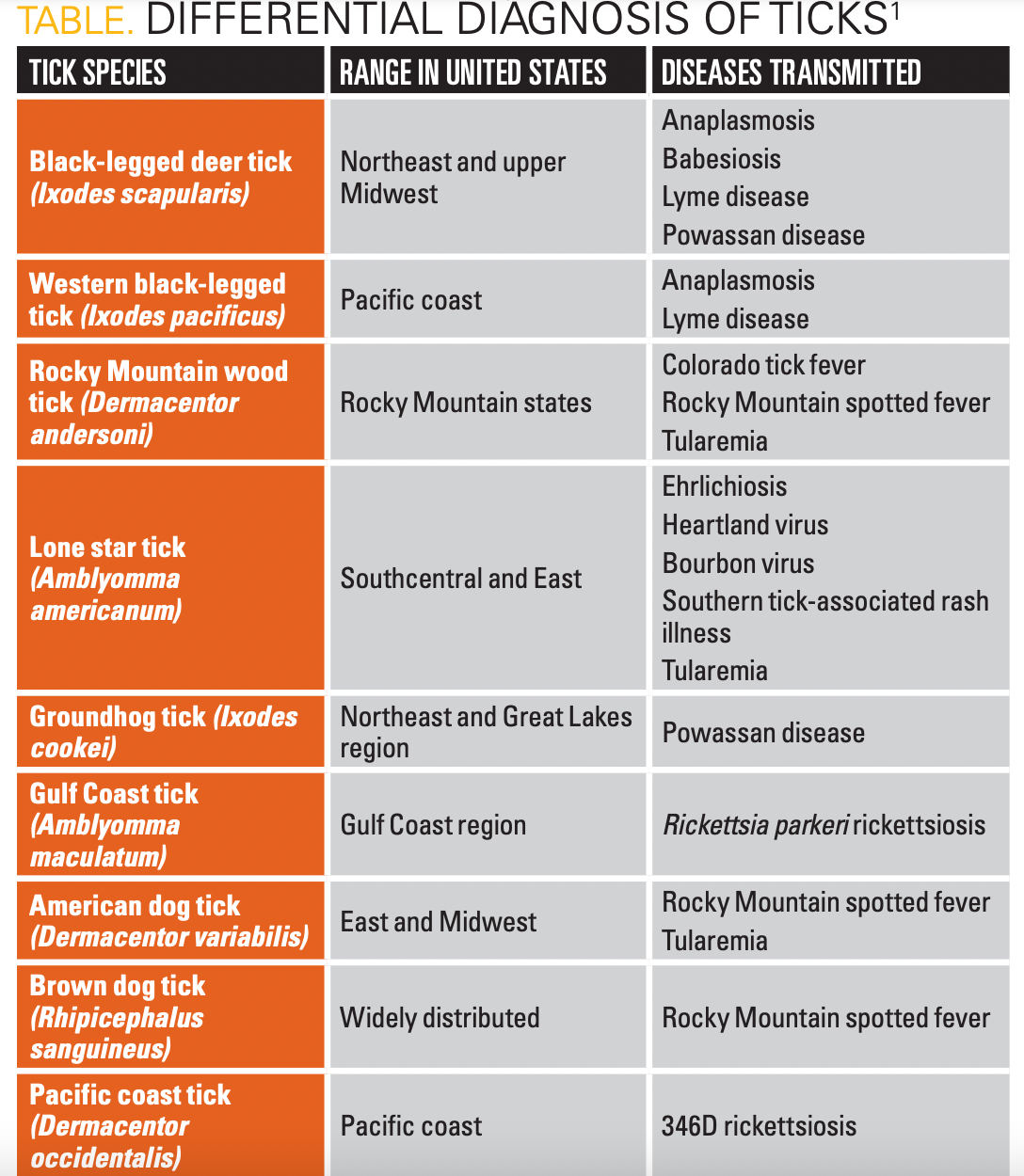
There are several tick species that can transmit a variety of diseases, listed in the Table.1
Based on the patient’s location, the most likely ticks are the black-legged tick, lone star tick (LST), groundhog tick, and American dog tick. Tickborne diseases cause several similar symptoms, including fever, muscle aches, fatigue, headaches, and rashes.2 The most distinguishing feature of this patient’s ticks is the white spot on its back, which points to the LST as the actual culprit.
Lone star tick
LSTs (Amblyomma americanum) are the most common human-biting ticks in the United States but are often overshadowed by deer ticks (Ixodes scapularis).3 They actively seek hosts and require 3 blood meals from 3 different hosts throughout their life cycle from larva to nymph to adult. Humans can serve as hosts at all 3 stages, and a bite from an LST at any stage leads to possible exposure to pathogenic agents.2 White-tailed deer are also important hosts for LSTs.4 Adult female LSTs have a characteristic white spot on the dorsal surface,5 and adult males have white streaks around the outer edge of the dorsal surface (Figure 1). LST bites present as erythematous papules, as seen in Figure 2, in both children and adults.
Geographic range
Although commonly thought of as being a Southern tick species, the LST has a large range extending north, as shown in Figure 3 from the CDC.6
Figure 3. Geographic Range of the Lone Star Tick6

Historically, the LST was seen as far north as New York and Michigan. With European colonization and the resulting clearing of vegetation, burning of forests, and deer hunting, the LST population decreased, particularly in the Northern states, with higher numbers in the South. In the past few decades, there has been a northward shift of the LST range, which could be due to several factors including climate change, expansion of the deer population, and reforestation of the northeast United States.4
The condition
LSTs have been associated with several bacterial and viral infections as well as red meat allergy. Research continuously adds to the list of diseases caused by the LST.
Bacterial
Ehrlichiosis is caused by the Ehrlichia bacteria. Symptoms include chills, fever, muscle aches, headaches, nausea, and vomiting. Serious complications include neurologic complications, respiratory failure, organ failure, and death.3 Doxycycline is the treatment of choice.7
Tularemia is caused by Francisella tularensis and can present with symptoms such as fever, enlarged lymph nodes, ulcers at the bite sites, sepsis, and meningitis.3 Streptomycin or gentamicin are recommended for treatment.6
Rocky Mountain spotted fever is caused by Rickettsia rickettsii. Fever, aches, nausea, and rash are symptoms.3 After 5 to 7 days, small pink macules that usually become purpuric and necrotic appear on the distal extremities and often disseminate. Treatment is with doxycycline.7
Southern tick-associated rash illness may be carried by LSTs, as the distribution of cases matches the geographic range of LSTs. It is similar to Lyme disease with an erythema migrans rash but has milder symptoms.3
Viral
LSTs are vectors for the Bourbon, Heartland, and Tacaribe viruses (Orthomyxoviridae, Phenuiviridae, and Arenaviridae families, respectively). Infection with these viruses in general causes fever, headaches, joint and muscle aches, and fatigue.3
Bourbon virus was first identified in Kansas. There have been 2 published reports of Bourbon virus. In addition to the flu-like illness, both reported adult patients had leukopenia with lymphopenia, thrombocytopenia, hyponatremia, and increased liver enzymes. Both deteriorated even after receiving doxycycline and passed away in the hospital.5
Heartland virus was first identified in Missouri but has also been seen in other Southern and Midwest states such as Oklahoma, Kansas, Arkansas, Tennessee, Kentucky, South Carolina, Georgia, Indiana, and Illinois. Along with influenza-like symptoms and lab abnormalities as described above, some patients also present with gait abnormalities, confusion, and dizziness. Severe cases may present with septic shock and multiorgan failure.5
Testing for these viruses is not readily available, so suspected cases should be reported to the state health department5; treatment is supportive.7
Alpha-gal syndrome (red meat allergy)
Red meat allergies following LST bites are due to sensitization to galactose-α-1,3-galactose (α-gal), an oligosaccharide found on mammalian red blood cells. Most patients with mammalian meat allergies have a history of tick bites. Allergy symptoms have a delayed presentation, often 2 to 10 hours after ingesting meat or relation-containing foods or medications. Sixty percent of patients present with anaphylaxis while the rest develop urticaria, angioedema, diarrhea, and abdominal pain. For diagnosis, total serum immunoglobulin E (IgE) and specific IgE levels to beef, pork, and lamb extracts can be analyzed to look for positive IgE reaction to α-gal. The treatment includes avoidance of all red meat, gelatin-containing products, and immunotherapy with cetuximab and infliximab. Allergic reactions should be treated symptomatically with antihistamines, corticosteroids, or subcutaneous epinephrine for anaphylaxis.6
Prevention
An important component of tick bite prevention is wearing protective clothing, including long pants tucked into socks, long-sleeved shirts, and light-colored clothing, which makes it easier to spot ticks. Insect repellant is also helpful, especially those containing DEET (diethyl-m-toluamide). Any ticks found on the body should be carefully removed with tweezers or other tick-removal devices to avoid crushing the tick or removing the mouthparts that inject saliva and pathogens.6
Patient course
The patient took doxycycline for 5 days for prophylaxis of Lyme disease, which she stopped when it was realized that LSTs are not a source of Borrelia species. She also took cefuroxime for 3 days for prophylaxis of ehrlichiosis. Her symptoms completely resolved in 21 days with no further sequelae.
Discussion
Despite being a common tick species with a large range extending over half of the eastern United States, the LST is not as well-known everywhere in its range. The LST, with its distinctive white spot on the back of females, is a vector for several bacterial and viral pathogens, including Ehrlichia, Tularemia, Rickettsia, Bourbon virus, Heartland virus, and Tacaribe virus. Bites from the LST can also lead to red meat allergy. Antibiotics are effective in the treatment of bacterial infections, but supportive care is the only option for viral infections.
In the case presented, the patient presented with numerous erythematous papules and later developed headaches, fatigue, rashes, and soreness, but no fever, after tick bites. She improved with prophylactic antibiotics. While the LST is not typically thought to be present in the Northeast, the presence of the white spot on the patient’s ticks helped identify it as the LST. Moreover, warming of the environment and regrowth of protected forests has most likely resulted in an increase in the population of LSTs, which increases the risk of LST bites especially in children who spend a lot of time outdoors hiking or playing in the woods. The LST is clearly an important tick species for pediatricians to keep in mind as they care for children who live and/or travel in the eastern United States.
Click here for more from the April issue of Contemporary Pediatrics.
References:
1. Diseases transmitted by ticks. CDC. September 11, 2023. Accessed December 1, 2023. https://www.cdc.gov/ticks/diseases/index.html
2. Symptoms of tickborne illness. CDC. August 5, 2021. Accessed December 1, 2023. https://www.cdc.gov/ticks/symptoms.html
3. Kennedy AC, Marshall E. Lone star ticks (Amblyomma americanum): an emerging threat in Delaware. Dela J Public Health. 2021;7(1):66-71. doi:10.32481/djph.2021.01.013
4. Rochlin I, Egizi A, Lindstrom A. The original scientific description of the lone star tick (Amblyomma americanum, Acari: Ixodidae) and implications for the species’ past and future geographic distributions. J Med Entomol. 2022;59(2):412-420. doi:10.1093/jme/tjab215
5. Higuita NIA, Franco-Paredes C, Henao- Martínez AF. The expanding spectrum of disease caused by the Lone Star Tick, Amblyomma americanum. Infez Med. 2021;29(3):378-385. doi:10.53854/liim-2903-8
6. Diaz JH. Red meat allergies after lone star tick (Amblyomma americanum) bites. South Med J. 2020;113(6):267-274. doi:10.14423/SMJ.0000000000001102
7. Rodino KG, Theel ES, Pritt BS. Tick-borne diseases in the United States. Clin Chem. 2020;66(4):537-548. doi:10.1093/clinchem/hvaa040

Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.