
Pediatricians need to recognize symptoms of perinatal depression in new mothers, provide basic counseling and treatment, and refer for appropriate services when needed.

Pediatricians need to recognize symptoms of perinatal depression in new mothers, provide basic counseling and treatment, and refer for appropriate services when needed.

A landmark observational study is the first to report on the effect of ultraviolet-free blue light therapy on allergic skin disease in newborns.

In my 40-plus years of pediatrics, I have sometimes treated patients based on the best of intentions, but with perhaps the worst of evidence. Here are some “best practices” I have used, and discarded, over time.

New research examined the potential role of Gram-negative skin bacteria in the pathogenesis and exacerbation of eczema, and their effectiveness to treat it.

Children with psoriasis may have higher rates of associated medical comorbidities. Newest recommendations say such kids should be screened for these risk factors.

Treatment of obstructive sleep apnea/nocturnal hypoxia with continuous positive airway pressure (CPAP) in children with nonalcoholic fatty liver disease (NAFLD) reduces the severity of liver injury and of oxidative stress.

The primary care physician needs to have in place appropriate strategies for evaluation of urologic issues and recommendations to parents who broach these topics.
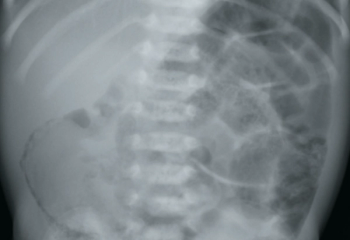
A 6-day-old, late-preterm male neonate presents to his pediatrician’s office with bilious emesis and is admitted for further evaluation. He was born at 36 weeks and 6 days via spontaneous vaginal delivery to a 23-year-old G4P4 mother with negative serologies, negative antenatal Group B Streptococcus testing, and no significant prenatal events. His stay in the newborn nursery was unremarkable. The neonate is exclusively breastfed, has no history of rectal bleeding, and passed meconium within the first 24 hours.

Tailoring drug delivery modalities to the individual patient based on age, ability level, and preference can optimize control of pediatric asthma.

When teenaged athletes complain of lumbar back pain that worsens with activity, there should be a high index of suspicion for a spondylolysis.

Pediatricians are quite capable of caring for both the physical and mental health of patients. Here is how embedding mental health services into your practice and collaborating with community mental health professionals can accomplish both.
Indeed it does, according to a randomized trial conducted during a 3-year period in England and Wales in more than 1300 exclusively breastfed infants.

The mother of a healthy 4-week-old boy brings him to the office for evaluation of a small pit on the medial canthus of the left eye, noted since birth. There is constant drainage of tears onto the left side of his face and exudate on the bottom of the left medial canthus.

Kids deserve the best care when they are ill or injured, and the best care should come from seeing the pediatrician in the medical home.