
Epilepsy
Latest News
Latest Videos
CME Content
More News

Elia Pestana Knight, MD; and Whitney Mitchell discuss how CDKL5 deficiency disorder affects children, and how ganaxolone (ZTALMY; Marinus) can drastically improve and even save lives.

A recent review highlighted potential methods of managing infantile epilepsies, including levetiracetam, ketogenic diet, modified Atkins diet, and surgery.

Since its approval for the treatment of medical refractory epilepsy in 2013, the closed-loop neuromodulation device has had its efficacy and safety confirmed in several pivotal studies and will now be assessed in focal epilepsy in the RESPONSE trial.
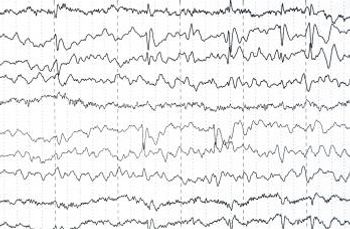
For monitoring epilepsy, long-term monitoring can be effective without requiring the time and cost of a hospital stay.

Examining 2 of the medications that can be used as an adjunctive treatment for epilepsy.
Telemedicine has been shown to be an effective way to provide care. A study examines its efficacy in managing epilepsy.

The US Food and Drug Administration (FDA) approves Fintepla (fenfluramine) through Priority Review.
Many hospitals see pediatric patients who present with seizures in the emergency department, but a majority of cases that require admission are transferred to other facilities.

In this expert Q&A, Julie Sherman, PhD and Jay Tarnow, MD briefly discuss the latest research findings on ADHD.

Autism spectrum disorders affect 1 in 100 children and the prevalence is 3 times higher in females. One-third of all children with autism have seizures.

Childhood absence epilepsy is distinct from partial epilepsy and is often misdiagnosed as ADD/ADHD. It is one of the most common types of pediatric seizure.

A third of patients with epilepsy are refractory to current treatment options. Thus, new agents are a welcome addition.

A 6-month-old boy with dysmorphic facial features, ear anomalies, and hypospadias brought for evaluation of elevated temperature and generalized seizure. Infant born at term to a 37-year-old mother via uncomplicated cesarean delivery.

ABSTRACT: Status epilepticus (SE) is associated with high morbidity and mortality in children. Fever is a common cause of SE and may precipitate seizures in children who have underlying epilepsy risk factors or may signal intracranial infection.

Four-month-old Hispanic boy brought for evaluation because of hypopigmented patches on his skin and a history of seizures. Infant was the product of an uncomplicated pregnancy; born at 40 weeks' gestation to a 16-year-old gravida 1, para 1 mother who received appropriate prenatal care. At birth, he had multiple hypopigmented patches on his face, torso, and extremities. At age 2 months, he was hospitalized for new-onset seizures.

It can be difficult to determine whether unusual, paroxysmal behavior represents a seizure or a nonepileptic event. Children with sudden flailing movements or unresponsive staring may, in fact, be experiencing psychogenic events.

This 4-year-old girl was born to a 27-year-old gravida, 1 para 0 mother at 37 weeks' gestation via vaginal delivery. The pregnancy was uncomplicated. Apgar scores were 8 at 1 minute and 9 at 5 minutes. The child's birth weight, head circumference, and length were 3045 g, 33 cm, and 50 cm, respectively. Her mother noted global developmental delays (particularly in the areas of speech and fine motor skills), abnormal sleep habits, obstructive sleep apnea, and seizure disorder. Family history was unremarkable.

ABSTRACT: Most cases of cerebral palsy (CP) are the result of congenital, genetic, inflammatory, anoxic, traumatic, toxic, and metabolic disorders. A minority of cases result from asphyxia at birth. Nearly three-quarters of children with CP aged 7 years had a normal neurological evaluation at birth. Abnormal motor development usually provides the first diagnostic clue. Neuroimaging is recommended if the cause of CP has not been established with perinatal imaging. MRI is preferred to CT. Management of the multisystemic manifestations begins with a comprehensive medical evaluation by a multidisciplinary team that includes family members. Therapy is aimed at maximizing the patient's level of function. Key areas include ambulation, cognitive skills, activities of daily living, hygiene, and rehabilitation into society.

ABSTRACT: Adolescent drivers with attention deficit hyperactivity disorder (ADHD) are more likely to be involved in--and to die of--a driving accident than any other cause. The higher occurrence of driving mishaps is not surprising given that the core symptoms of ADHD are inattention, impulsivity, and hyperactivity. Safe driving habits can diminish the risk, however. The first step is to inform patients of the dangers of driving; the significance of adolescence, ADHD, and medication can be underscored in a written "agreement." Strategies to promote safer driving--especially optimally dosed long-acting stimulant medication taken 7 days a week--may be critical. A number of measures lead to safer driving by reducing potential distractions during driving (eg, setting the car radio before driving, no drinking or eating or cell phone use while driving, no teenage passengers in the car for the first 6 months of driving, and restricted night driving).

How long should I keep giving anticonvulsant medications to a child with benign genetic epilepsy?

Steven, a 13-year-old boy, experienced his first headache at age 7 years. The frequency, intensity, and duration of his headaches have been increasing over the past 6 months. Steven now experiences 7 to 10 headaches each month that last up to 8 hours. The headaches are associated with mild nausea, light and sound sensitivity, dizziness, fatigue, occasional abdominal discomfort, and difficulty in concentrating. Last year, he had a vomiting episode because of a headache. The pain is usually more prominent in the forehead and does not favor either side of the head. The headaches usually begin in the morning before he leaves for school. As a result, Steven has missed nearly 25% of his school days this semester; his parents are considering home tutoring for "sick children who are unable to attend school."

Attention deficit hyperactivity disorder (ADHD) is very common. In the United States, between 6% and 10% of children and adolescents are affected, as are 4% of adults.1 Children in other countries also have ADHD, although rates of comorbid disorders may vary from those found in the United States.2

During a routine physical examination, a 3-year-old boy was noted to have speech delay and hyperactive behavior. The child was born at term to a 25-year-old mother with epilepsy, which was managed with phenytoin. His birth weight was 3.5 kg (7.8 lb); he had no neonatal problems or features of fetal Dilantin syndrome. However, he had undergone bilateral hydrocele and inguinal hernia repair and tube placement for recurrent ear infections. His half sister (from his mother's previous marriage) needs help in reading and math. His father is healthy.

A 9-year-old girl presents with multiple hyperpigmented lesions, some of which have been present since birth (Figure 1). The lesions have increased in size and number. There is no history of seizures. Her 40-year-old mother has multiple skin nodules (Figure 2).

During a neurologic evaluation for seizures, a 17-year-old boy with epilepsy was noted to have a deformity of both lower eyelids. According to the boy's mother, the deformity had been present since birth; it was not related to the patient's neurologic condition.








