Recurrent nausea and vomiting in an 18-year-old
Can you guess the diagnosis?
Case
This 18-year-old female was diagnosed in early childhood with Goldenhar syndrome (oculo-auriculo-vertebral syndrome). She has a history of congenital D-transposition of the great vessels status post repair, right ventricle pulmonary artery conduit, cardiac ablation for arrhythmia, developmental delay, and melody valve. She underwent menarche at age 13, with irregular menses about one to two times a year, which were increasingly painful. At age 16, she had a pelvic ultrasound suggestive of an ovarian cyst, and she was advised on expectant management. At age 18, she initially presented with severe abdominal pain and vomiting, prompting a visit to urgent care from which she was discharged.
Four weeks later, the patient presented to a local emergency department with recurrence of severe nausea, vomiting, and abdominal pain. Initial vital signs in the emergency department showed temperature 36.2°C, pulse 94 bpm, respirations 18, SpO2 99%, and blood pressure 186/110. The urine sample showed no obvious infection. White blood cell count (WBC) was elevated at 14.35. A CT scan was performed, which showed the following findings (Figure 1):
- Mullerian duct anomaly with a right hemiuterus and a rudimentary left cavity. There is fluid distention of the left rudimentary cavity measuring up to 3.2 cm.
- Tubular cystic structure in the left adnexa compatible with hydrosalpinx. Consider further evaluation with pelvic ultrasound.
- Multiple metallic densities in a linear distribution within segments 4A and 4B in the left hepatic lobe anteriorly with adjacent periportal hypoattenuation, presumably secondary to prior intervention such as prior embolization.
- Partially imaged cardiomegaly.
The patient was discharged after symptoms improved with antiemetics and pain medications.
The following day, the patient presented to a different emergency room with a temperature of 36.7°C, heart rate 97, SpO2 96%, respirations 24, and blood pressure 166/98. WBC had increased to 16.3. C-reactive protein was 1.0. Basic metabolic panel and procalcitonin were within normal limits. At this time, due to abnormalities on EKG, she was admitted to the cardiology service overnight for monitoring in the setting of her surgically repaired congenital cardiac anomaly. She was discharged the following day.
Further evaluation
A month later, she presented to the emergency department again with recurrence of severe nausea and vomiting without abdominal pain. A transvaginal ultrasound was attempted but not tolerated by the patient. An MRI abdomen and pelvis again demonstrated an obstructed rudimentary left uterine horn with severe distention of the left uterine cavity with blood products. Follow-up with gynecology was recommended, and the patient was discharged with a prescription for continuous combined oral contraceptive pills to take until gynecologic care was established (Figure 2).
Two weeks later, she was seen by a primary care physician, at which time she reported ongoing pain and nausea and had not taken her prescribed hormonal contraception. Subsequently, she presented to the local emergency department with nausea, vomiting, and severe abdominal pain. The images were reviewed by a gynecologist at a tertiary academic center via transfer center call per family request. Prompt referral to pediatric and adolescent gynecology was coordinated for surgical management, and the patient was started on norethindrone acetate for menstrual suppression.
Actual diagnosis
Obstructed left Mullerian remnant with significant inflammation and hematosalpinx, with a separate right unicornuate uterus and single vagina.
Management and patient course
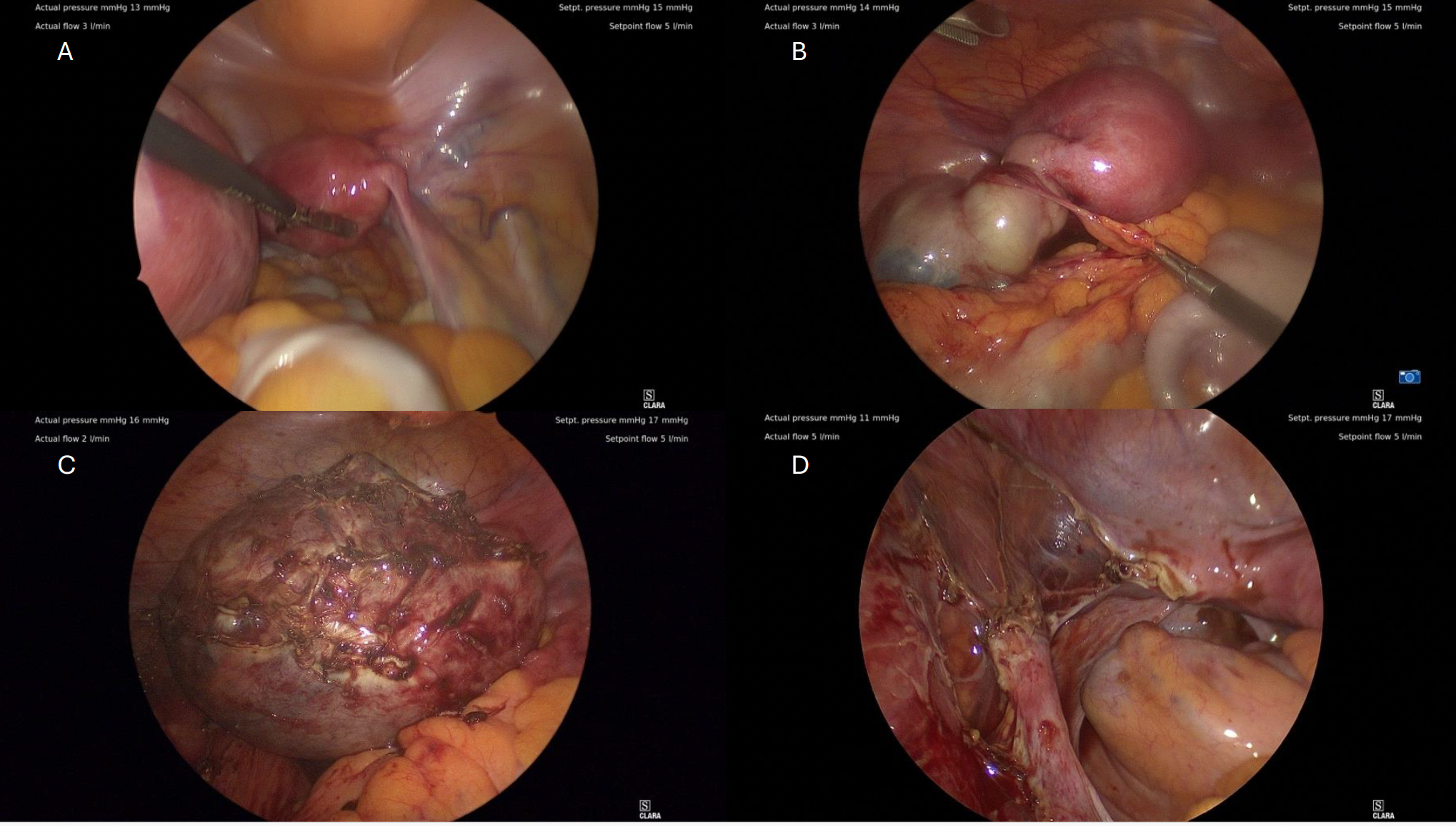
Figure 3. A) Right unicornuate uterus visualized at laparoscopy. B) Left obstructed horn with distended adnexal structure and omental adhesions. Note the smaller right unicornuate uterus in the background. C) Left obstructed horn after separation from surrounding structures. The adnexal mass was separately excised. D) Post-excision appearance of pelvic side wall. The right unicornuate uterus can be seen in situ.
Definitive surgical management was performed via laparoscopy with supracervical laparoscopic excision of Müllerian remnant and left salpingectomy. After placement in a laparoscopic containment bag, the excised Müllerian horn was hand morcellated at the umbilical incision for extraction. The right unicornuate uterus was inspected and appeared contiguous at the level of the cervix but was otherwise separate and unaffected, and left in situ. Pathology confirmed excision of the left tube and uterus; no separate definitive ovarian tissue was noted.
Following surgery, norethindrone acetate was prescribed, but due to mood side effects, the patient elected to discontinue the medication and resumed regular menstrual cycles without dysmenorrhea.
The patient’s pain resolved within 4 days of surgery, and at follow-up, she continued to do well with the return of her menstrual cycle. She plans to continue her routine care with her primary care physician close to home.
Discussion
Goldenhar syndrome (oculo-auriculo-vertebral syndrome) was first described in 1952 with ophthalmic, auricular, and facial features, with additional associations having been added in more recent descriptions. The additional features include vertebral, cardiac, renal, and neural anomalies.1 One previous publication reported an association with Mullerian agenesis, but no other anomalies of the Mullerian tract have been reported.2 In this patient, Goldenhar Syndrome presented with craniofacial microsomia with left microtia, aural atresia, facial asymmetry, and hearing loss. Ipsilateral facial underdevelopment and external ear anomalies are considered a notable association for Goldenhar syndrome.3,4 Case reports note the increased prevalence of ipsilateral pulmonary involvement, such as agenesis, being more common than contralateral involvement.5,6 The aural atresia and microtia in this patient occurred ipsilateral to the uterine horn remnant. Future research is suggested to assess the genetic or developmental plausibility of associations.
Goldenhar syndrome has previously been associated in a case report with complete Mullerian agenesis, but has not been described in connection with other Mullerian anomalies, such as an obstructed uterine horn remnant seen in this case.2 This patient was evaluated several times with imaging findings suggestive of obstructive remnant; however did not present to gynecologic care for several months, as other differential diagnoses, including gastroenteritis and cardiac etiologies, were emphasized in light of the patient’s medical history. Diagnosis in this case was hindered by a lack of continuity of care due to the variety of places the patient was seen, including PCP, multiple emergency departments, and urgent care. Additional barriers included inconsistent history and symptom identification attributed to the patient’s developmental delay, and difficulty in accessing pediatric and adolescent gynecologic subspecialty care. This case highlights the importance of considering Mullerian anatomy in individuals with Goldenhar syndrome and the general population to ensure that an obstructive menstrual egress is appropriately treated in a timely manner.
References
- Bogusiak K, Puch A, Arkuszewski P. Goldenhar syndrome: current perspectives. World J Pediatr. 2017 Oct;13(5):405-415. doi: 10.1007/s12519-017-0048-z.
- Benjamin JC. Goldenhar syndrome associated with genital tract abnormality. BMJ Case Rep. 12(8):e230686. Aug 28, 2019. Doi:10.1136/bcr-2019-230686
- Goswami M, Bhushan U, Jangra B. Goldenhar Syndrome: A Case Report with Review. Int J Clin Pediatr Dent. 2016;9(3):278-80. doi:10.5005/jp-journals-10005-1377
- Vinay C, Sudhakara Reddy R, Uloopi KS, Madhuri V, Chandra Sekhar R. Craniofacial features in Goldenhar syndrome. Journal of Indian Society of Pedodontics and Preventive Dentistry 27(2):121-4, Apr–Jun 2009. doi: 10.4103/0970-4388.55339
- Bedi M, Jain RK, Barala VK, Singh A, Jha H. A Constellation of Rare Findings in a Case of Goldenhar Syndrome. Case Rep Pediatr. May 21, 2017. doi:10.1155/2017/3529093
- Utkarsh S, Sharma P, Tyagi H, and Nischal N. The “expanded Goldenhar syndrome” – A rare entity. Case Rep Clin Radiol. March 6, 2024. doi: 10.25259/CRCR_6_2024
Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.