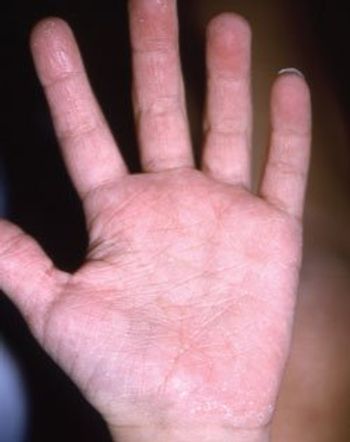
A 6-year-old boy has a rash on his hands and feet that erupted shortly after he startedfirst grade. His parents are concerned that he may be allergic to something at school, such as chalk. He is otherwise healthy.
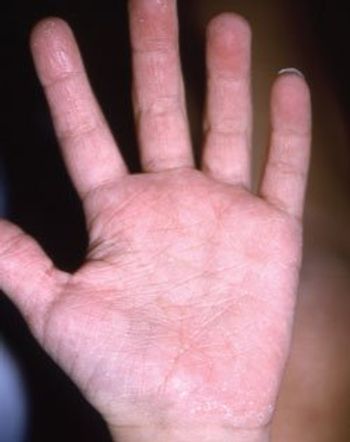
A 6-year-old boy has a rash on his hands and feet that erupted shortly after he startedfirst grade. His parents are concerned that he may be allergic to something at school, such as chalk. He is otherwise healthy.

Severe disability and even death can result from the inappropriate diagnosis and treatment of a young child's wheezing, which is heterogeneous in its origins and expression. Consequently, a differential diagnosis is necessary to determine the cause and to develop an effective management strategy. Viral-induced wheeze, especially from respiratory syncytial virus (RSV), manifests as a bronchiolitis. Recent reports show that the cysteinyl leukotrienes are an important mediator of the airway effects of RSV infection and that leukotriene receptor antagonists reduce postrespiratory syncytial virus lung symptoms. Exercise-induced bronchoconstriction manifests as wheezing and can be treated or pretreated short-term with inhaled bronchodilators or cromolyn: long-term therapy includes inhaled corticosteroids and leukotriene receptor antagonists. Allergic rhinitis-associated wheeze may be the result of acute exposure to an allergen or simply from nasal dysfunction. Control of allergic rhinitis with intranasal steroids, antihistamines, or leukotriene receptor antagonists could relieve the wheezing. Asthma-associated wheeze requires long-term use of 1 or more daily controller medications. The primary goal is to navigate the child safely through the first episode of wheezing, consider the causes of the wheeze, and then evaluate the need for further therapy. All apparent causes of wheeze should be treated with the idea that if the apparent cause turns out not to be the actual cause, treatment can be safely discontinued.

With the introduction of Gardasil--the vaccine that protects against infection with human papillomavirus (HPV) types 6, 11, 16, and 18--pediatricians are fielding an increasing number of questions from parents about this disease. Parents want to know how prevalent HPV infection actually is and how much of an impact the vaccine will have.

Oral contraceptive (OC) pills are frequently prescribed for a variety of clinical purposes. These medications--which contain varying amounts of estrogen- and progestin-based compounds--essentially "override" a woman's innate hypothalamic-pituitary-ovarian axis and frequently help ameliorate the effects of a maturing reproductive system while preventing pregnancy.

A 2-year-old girl was seen by her pediatrician because of a 3-day history of runny nose, cough, congestion, and low-grade fevers. A viral upper respiratory tract infection was diagnosed and supportive care was recommended. The child returned 2 days later with persistent cough, mild tachypnea, and an episode of vomiting. The cough and tachypnea prompted the pediatrician to order a chest film, which revealed an enlarged cardiac silhouette.

Several hours before he was seen in the office, a 2-year-old boy passed stool that contained a large intact sunflower seed. He had poor appetite and abdominal cramps but no recent history of emesis or fever.

This young girl is brought to your office with a rash that her mother thinks is triggered by sunlight. The mother is concerned because her own aunt has lupus erythematosus. The mother also reports that several children at her daughter's school have a similar eruption.

A 16-month-old Hispanic girl presented with a 2-day history of pain, redness, and swelling of the left side of her groin. Her mother first noticed the lesion after the child was seen limping and scratching the area. The mother thought her child had been bitten by an insect but did not witness any bite.

In the February 2007 issue (Photo Quiz, page 88), there is a case of a child with a rash diagnosed as erythema multiforme (EM) rather than urticaria. I assume that these were fixed lesions, which distinguished them from urticaria lesions? Also, if this rash had been caused by the antibiotic the patient had been taking for an acute otitis media infection, why did it first manifest after 4 days of treatment?

A well-nourished 17-year-old of average height and weight was referred for evaluation of persistent right lower leg pain of 3 months' duration. He was not taking any medications, had no allergies, and denied trauma to the area.

I read with interest the Dermclinic case on molluscum contagiosum in your February issue. I was a bit surprised by the last sentence, in which Dr Barber comments, "I often instruct affected young adults to pierce the top of the lesions and try to extrude the central core using lateral pressure with the rounded end of a popsicle stick or similar device . . ."

A 13-year-old boy presented with marked periorbital swelling of the left eyelid that started 12 hours earlier. His eyelashes and lid were matted with yellow discharge. He did not wear contact lenses or eyeglasses and denied ocular trauma or foreign bodies. He had been nauseated and vomited once; his mother attributed these symptoms to an antibiotic he had been taking for 5 days for a sinus infection. The medical history was noncontributory; there was no family history of ocular problems.

A 12-year-old girl was brought by her parents for evaluation of a spot in her eye, which they feared might be an embedded foreign body. She had nominal eye discomfort, which was probably secondary to attempted removal of the object. The child could not recall having dust particles in the eye, and she had no previous eye lesion.

The pearly papules on the cheeks (A), ear, and scalp (B) of 2 newborns are classic presentations of milia. The white or yellow papules range from 1 to 2 mm in diameter. They result from retained keratin and sebaceous material in pilosebaceous skin. The lesions commonly affect the face and may be present at birth or develop within the first few days of life.

This 17-year-old presented with multiple boils in the perineum and under breast and skin folds. The lesions produced a malodorous discharge (which caused problems with peer acceptance at school) and were increasing in size. Oral antibiotics had not helped. The patient was admitted for intravenous antibiotic therapy.