
Treatments for cystic fibrosis are evolving. Here’s a look at new CFTR modulator therapies including the most recent approval-elexacaftor/tezacaftor/ivacaftor (Trikafta).

Treatments for cystic fibrosis are evolving. Here’s a look at new CFTR modulator therapies including the most recent approval-elexacaftor/tezacaftor/ivacaftor (Trikafta).

Pediatricians need to implement the strategies of assessing, adjusting, and reviewing symptoms and risks of severe asthma to confirm the diagnosis and implement appropriate interventions.

Using palivizumab in infants with cystic fibrosis (CF) may not lead to long-term improvements, according to a new study published in Pediatrics. Researchers used the Cystic Fibrosis Foundation Patient Registry data.

Certainly, these are interesting times in medicine as the integration of homeopathic remedies and over-the-counter supplements has become increasingly more common in the past few decades. However, with inconsistent medical research and a lack of US Food and Drug Administration regulation, it remains unclear what the most safe and efficacious role these substances will play in the future of medical care.

Severe or refractory asthma places a small subset of children with asthma at risk for significant morbidity and treatment challenges, as well as for higher healthcare utilization and costs.

Patients with cystic fibrosis (CF) are deficient in vitamin D, which at higher levels can help prevent exacerbation. A new study examines current guidelines and future recommendations.

Tailoring drug delivery modalities to the individual patient based on age, ability level, and preference can optimize control of pediatric asthma.

Asking a series of questions that can lead to more appropriate preventive medication use can go a long way in improving the health of children with asthma and reduce hospitalizations.

Wheezing in children is often associated with asthma. However, localized wheezing should alert the clinician that something other than asthma may be present.

For Contemporary Pediatrics, Dr Bobby Lazzara discusses a recent prospective birth cohort study published in Pediatrics that looked at different feeding methods for infants and whether the methods had any link to asthma.
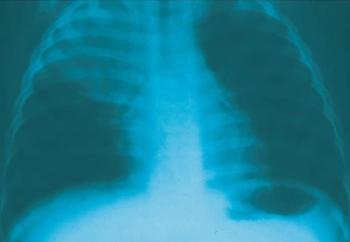
Respiratory symptoms are a major reason why outpatients seek medical care, and primary care physicians who treat children frequently see pneumonia. This week’s photo essay tests your knowledge of respiratory problems in kids.

Although bronchiolitis is commonly seen in very young children, the infection can be dangerous and even fatal for some infants. Here, new thoughts on risk factors that may determine which babies get very sick.

Hoarseness developed in a 27-month-old girl who was previously treated in the ED for a presumed asthma exacerbation and bronchiolitis.

A 6-month-old boy with 1-week history of dry cough that worsened at night. He had been wheezing off and on for the past month and had visited the emergency department on one occasion.




A 3-month-old African American boy was referred for evaluation of poor weight gain and vomiting. The infant had been evaluated by his primary care physician 15 times within the past 6 weeks; he had no change in symptoms despite various treatments.

A 2-month-old boy is brought to the emergency department (ED) because of “noisy breathing” that has been present since birth. The parents report that they occasionally see the child’s ribs during inspiration when he is lying down.

Tuberculosis (TB) remains one the most important infectious diseases in the world. More than 8 million people are infected every year. The vast majority of infections--95%--occur in developing countries, where the disease accounts for 25% of avoidable adult deaths.

Day-old boy born at term via vaginal delivery complicated by shoulder dystocia. He had very mild cyanosis in the extremities at birth, which resolved after 5 minutes. Referred for evaluation of respiratory distress. Birth weight, 3.3 kg (7.4 lb). Apgar scores: 7 at 1 minute, and 9 at 5 minutes.

Pneumonia is one of the most common conditions encountered by primary care providers. Certain organisms cause pneumonia in particular age groups. For example, group B streptococci, Gram-negative bacilli Escherichia coli in particular) and, rarely, Listeria monocytogenes cause pneumonia in neonates. In infants younger than 3 months, group B streptococci and organisms encountered by older children occasionally cause pneumonia, as does Chlamydia trachomatis. Older infants and preschoolers are at risk for infection with Streptococcus pneumoniae and Haemophilus influenzae. In children older than 5 years, S pneumoniae and Mycoplasma pneumoniae are the key pathogens. Let the patient's age, history, clinical presentation, and radiographic findings guide your choice of therapy. Even though most patients with uncomplicated pneumonia can be treated as outpatients, close follow-up is important. Hospitalize patients younger than 6 months and those with complications.