
Three profiles of a magical waste basket, a reusable breastpump, and a t-shirt that helps prevent food allergies.


Three profiles of a magical waste basket, a reusable breastpump, and a t-shirt that helps prevent food allergies.

Teen with painful papules and plaques is diagnosed with Sweet's Syndrome

The ninth in a year-long series of commentary reviewing topics published in Contemporary Pediatrics 25 years ago. This month's article reviews the causes and management of hirsutism in adolescent girls.
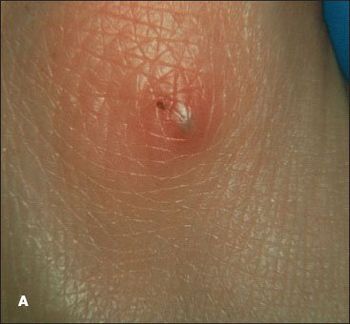
Purpuric pustules can present diagnostic challenges. However, the ability to correctly identify these lesions can be of crucial-even lifesaving-importance in caring for ill children.

Erythematous pustules and papules with some coalescence developed on the anterior trunk and to a lesser degree on the face and extremities of a newborn boy the day after birth. The baby was born at full term after an uncomplicated pregnancy and delivery.

An apparently healthy 9-year-old girl noted to have left ankle mass during well-child checkup. Her last well-child visit was 3 years earlier. Medical history unremarkable. She denied fevers, weight loss, night sweats, and chills. No family history of bone deformities or growth disturbances.

Few clinical scenarios engender as much anxiety as the sudden onset of rash and fever in a child. However, the diagnostic possibilities can be quickly narrowed-and the likelihood of potentially serious disease can be assessed-with a triage system that involves classifying the presenting symptoms into 1 of 3 groups.

A 10-week-old white baby girl with a history of difficulty in breathing presented with stridor, tachypnea, wheezing, and increased work of breathing.

A child is born with congenital melanocytic nevi.

A 3-year-old boy with white patches on the trunk first noticed shortly after birth.

A 17-year-old girl presented for evaluation of right hip pain. Several months earlier she had incurred a twisting injury to her hip when she landed from a jump while dancing.

Episodic right-sided facial flushing was noted in a 2-month-old girl born at full term via forceps-assisted vaginal delivery. The erythema appeared within minutes of latching onto her mother’s breast and resolved within 5 to 10 minutes after breastfeeding. The episodes of flushing had begun a week before the clinic visit; there were no collateral symptoms of anaphylaxis. Because food allergy was suspected, the mother had eliminated all dairy products from her diet.

A 7-year-old boy was brought for evaluation of a nonpruritic, nonpainful, evolving polymorphic rash that began on the torso and spread to the extremities, face, palms, and soles over a 2-week period. He had been otherwise healthy and had no history of constitutional symptoms.

Circumscribed erythematous lesions developed on the back and abdomen of this 19-month-old boy. The rash was mildly pruritic. The parents gave the child 1 dose of diphenhydramine, and the rash resolved after an hour. About 12 hours later, new lesions developed on the face, neck, and upper back. The child was given the same treatment and the symptoms resolved. The following morning, widespread lesions were noted on the child's face, neck, trunk, and extremities.

It was hit by two hurricanes in September 2008 -- one literal and one financial -- but the Shriners Hospital for Children in Galveston will be reopening.

A 7-month-old child appears at the derm office with a blistering eruption that started six days before on her face and neck, and has spread to trunk and extremities.

The parents of this 6-year-old girl expressed concern about a yellow-brown arciform plaque on their daughter's cheek that has been present since birth. Although it has remained stable throughout her early childhood, her parents wonder whether it may become cancerous later on. Would you recommend removing the lesion?

Although it has been more than 40 years since Kawasaki disease was first described, it is still something of a medical mystery.

In his Dermclinic case in the March 2009 issue of CONSULTANT FOR PEDIATRICIANS (page 77), Dr Kirk Barber discusses juvenile plantar dermatosis (JPD). A very simple treatment for this condition is the use of a home foot spa, in which wax is melted and the foot immersed according to the directions included with the device. Following the wax immersion procedure, the patient should apply a good lotion. JPD can be remedied or at least controlled with this treatment.

A 5-month-old Asian boy was brought for evaluation of hair loss and a red, scaly rash on the scalp and body. The rash had not responded to hydrocortisone 2.5% ointment. There was a family history of asthma, food allergies, and allergic rhinitis. His mother had Hashimoto thyroiditis.

Asthma exacerbations continue to cause a significant number of emergency care visits and hospitalizations among children.1 In “Managing Asthma in Children, Part 1” (CONSULTANT FOR PEDIATRICIANS, May 2009, page 168), we reviewed the epidemiology, risk factors, and diagnosis of asthma in children. We also discussed how to make an initial assessment of asthma severity. In Part 2, we review the key components of treatment.

This white patch in the medial periorbital area of a 15-year-old girl had been present for several months. It was asymptomatic. The patient denied having had an injury to the area. Results of a potassium hydroxide preparation of a skin smear and fungus culture were negative. She had no history of other hypopigmented lesions and was otherwise healthy. There was no family history of vitiligo or autoimmune disease.

An itchy rash developed around the nose in this 8-year-old boy. At first it responded to the application of a midstrength corticosteroid cream. However, the rash returned promptly after the cream was stopped and then spread to the perioral area. It is no longer responding to treatment with the topical corticosteroid that initially was effective.

A 5-month-old girl with progressively worsening generalized rash of 3 weeks’ duration. No obvious sensitivity, fever, recent infection, medication use, or known contact with irritant.

A 14-year-old girl with systemic lupus erythematosus (SLE) was evaluated for worsening left leg pain of 1 week’s duration. A month earlier, she had presented with left knee arthritis and a vasculitic rash; the antinuclear antibody titer was positive. In addition, she had leukopenia, myositis, hypocomplementemia, and mild proteinuria.