
An 8-year-old girl presents with a 1-year history of the progressive development of multiple 5- to 8-mm hypopigmented macules all over her body. Her parents do not recall any other skin changes, and no other skin changes are evident on presentation.

An 8-year-old girl presents with a 1-year history of the progressive development of multiple 5- to 8-mm hypopigmented macules all over her body. Her parents do not recall any other skin changes, and no other skin changes are evident on presentation.

A 3-month-old African American boy was referred for evaluation of poor weight gain and vomiting. The infant had been evaluated by his primary care physician 15 times within the past 6 weeks; he had no change in symptoms despite various treatments.

Selective IgA deficiency (SIGAD) is the most common immunodeficiency disorder; it affects about 1 in 200 to 900 persons. Most affected children are asymptomatic.

A 5-ft 1-in, 183-lb 14-year-old girl was concerned about the areas of thickened hyperpigmentation on her posterior neck and in her cleavage.
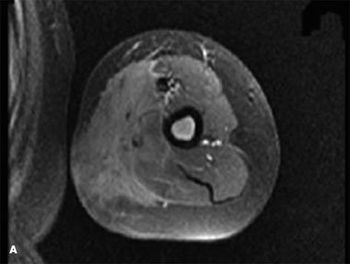
For 3 months, a 9-year-old boy had swelling of the left upper arm. An MRI scan obtained at another facility 1 week after onset showed extensive edema of the soft tissue at the midhumeral level. Laboratory results, including complete blood cell (CBC) count and Lyme titer, were normal.

A mother seeks an evaluation of her 20-month-old son, who has grown slowly and has had leathery dry skin since birth. He also has had multiple skin infections and chronic conjunctivitis, and he has delayed language development.

A 2-month-old boy is brought to the emergency department (ED) because of “noisy breathing” that has been present since birth. The parents report that they occasionally see the child’s ribs during inspiration when he is lying down.

Two girls present with toenail yellowing and thickening. What clinical clues will help you determine which toenails are mycotic?

The areas of hyperpigmentation shown here on the trunk of a 15-year-old girl appeared 2 years earlier as 1- to 2-mm hyperpigmented papules with either flat or verrucous surfaces.

A 5-year-old girl presented with a 2-day history of a widespread pruritic rash that began while the family was on vacation. The rash appeared suddenly as small pink macules and progressed to papules and pustules. Her brother had a similar-appearing but milder rash. She denied fever, chills, or constitutional symptoms. On further questioning, her father reported that she and her brother had been in a hot tub at their vacation home.

An 11-year-old boy with 4-month history of acnelike rash on his face and both upper arms. Rash is associated with redness and itching. Application of adapalene gel resulted in no change.

A 6-year-old girl has peeling soles on her feet. Although the peeling is not usually symptomatic, her feet become cracked, fissured, tender, and occasionally infected during the middle of the winter and summer.

An itchy eruption puts a damper on a girl’s Hawaiian vacation. How might you help her avoid a similar experience on her next trip to the tropics?

An 11-year-old girl presents to the clinic with a lesion under the tongue of 3 weeks' duration. She complains of a "mass sensation" while eating and speaking but has no difficulty with swallowing.

A 10-month-old breast-feeding boy was taken to the emergency department (ED) with a temperature of 40°C (104°F). Because he was on day 7 of treatment with amoxicillin for a previously diagnosed ear infection, unresolved otitis media was diagnosed.

One week earlier, a 14-month-old girl with a history of eczema was evaluated because of a diffuse rash of excoriated lesions, some of them purulent. She was afebrile. Worsening eczema with secondary infection was diagnosed. Treatment with oral clindamycin was prescribed. At follow-up, the lesions had worsened. The child had multiple excoriated papules, some of which had coalesced into plaques. She also had two 5-mm vesicles on her right shoulder. Eczema herpeticum was diagnosed clinically. Culture of the vesicles later grew herpes simplex virus (HSV).

The mother of this 4-year-old boy is concerned about a small drop of fluid that she noticed on her son’s neck at the dinner table the night before.

An adolescent girl seeks medical advice for managing recurrent nodules on her ear lobes. The diagnosis is keloids.

These hypopigmented, mildly pruritic lesions on the right arm of a 7-year-old African American girl appeared several weeks ago. She had no other lesions and was otherwise healthy. The diagnosis on the basis of the clinical presentation was lichen striatus.

This palpable, nontender, nonblanching rash had developed on the elbows of an 18-year-old boy and spread to the ankles and feet. The rash was accompanied by moderate abdominal pain associated with episodes of nonbloody emesis that did not change with eating or bowel movements. Diffuse joint pain developed the day after the rash appeared.

Intensely itchy, hyperpigmented macules developed on the shoulders and upper arms of a 16-year-old boy 2 weeks after he completed his eighth cycle of chemotherapy with bleomycin, etoposide, and cisplatin, following an orchiectomy for a stage IV germ cell tumor of the left testis. During the next 3 days, the lesions evolved into a papulopustular rash that spread to the upper chest, abdomen, and neck.

A 12-month-old awakens with asymptomatic juicy red papular eruptions on her cheeks. It is diagnosed as Gianotti-Crosti Syndrome.

The skin lesion pictured here is noted in a 12-year-old boy. His parents state that it developed when he was 1 year of age and that it has been growing with him ever since, with the number of “speckles” seen throughout the light brown background gradually increasing.

Because of the presence of unusual skin findings, a 3-year-old African American girl was evaluated for possible child abuse. The father, the primary guardian, reported that his daughter had returned home from her mother's residence 2 days before-a day earlier than planned. According to the father, the child was crying and had skin lesions, which initially appeared white and then darkened over the course of the next day or two.

A 5-year-old boy was brought for evaluation of ongoing thrombocytopenia before undergoing adenotonsillectomy for obstructive sleep apnea. The child had been given a diagnosis of "growing pains" after frequent evaluation for leg pain over the past 2 years.